INTRODUCTION
Management of distal radius fractures has been an ongoing evolution since Colles first described the injury in 1814.1 Operative treatment of these fractures has increased with a notable trend toward using volar plating.2,3 However, one reported complication associated with volar plate fixation is extensor tendon irritation or rupture. Because the extensor tendons rest against the dorsal cortex of the distal radius, even the slightest screw protrusion can injure a tendon. Numerous case reports and retrospective studies have shown that tenosynovitis or tendon rupture is caused by prominent screws extending beyond the dorsal cortex. Yet, there is a lack of clear consensus on identifying and preventing this complication.4–8 Thus, the incidence of extensor tendon complications due to surgical fixation of the distal radius remains at an estimated 2-6%.9–11
Further investigation of the distal radius anatomy has demonstrated high anatomic variability in this area.12–14 The geometric shape of the dorsal distal radius is complex, and standard intraoperative fluoroscopy may fail to reveal necessary details of anatomy. In addition, the dorsal cortex is often comminuted with fractures, making accurate screw length measurements even more difficult.
The purpose of our study is to further describe the anatomy of the dorsal ulnar aspect of the distal radius with attention focused on a sulcus that can hide dorsal screw penetration. We believe a better understanding of this anatomy will lead surgeons to have fewer tendon complications associated with screw penetration in volar plating procedures.
METHODS
We initially reviewed 64 consecutive magnetic resonance images (MRI) of the wrist. The images were obtained with a 1.5 Tesla strength scanner, and the thickness of each slice was 3.0 mm. We excluded five MRIs for any of the following reasons: incomplete imaging, skeletal immaturity, fracture of the radius, infection, or tumor, resulting in 59 MRIs for further evaluation. Using axial views, the dorsal aspect of the distal radius located ulnar to Lister’s tubercle called the “dorsal ulnar blind spot,” was evaluated. The axial cut of each MRI that displayed the maximum sulcus depth was utilized for measurement. A line was drawn from the apex of Lister’s tubercle to the dorsal ulnar corner of the radius [Figure 1]. From this line, a perpendicular line was drawn to the deepest point in the sulcus and recorded as sulcus depth. The distance of the radiocarpal joint was also documented for the selected axial image by utilizing scout line mode to establish a coordinate in the mid portion of the radius on the sagittal image. The coordinate was used as an origin and measured perpendicularly to the edge of the radius at the lunate fossa. An orthopaedic surgery and radiology resident reviewed all wrist images, and a single measurement was recorded between the two. Measurements were rounded to the nearest 0.1 mm, and a Student t-test was used to determine the statistical significance of sulcus depth and radiocarpal joint between gender and wrist laterality, with a P-value < 0.05 considered significant.
RESULTS
We evaluated the dorsal ulnar aspect of the distal radius using wrist MRIs consisting of 33 females and 26 males. Additionally, using the data gathered, we reduced our dorsal tendon irritation incidence rate from 2% (3/163) to 0% (0/151).
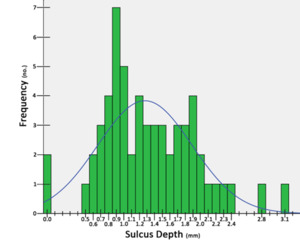
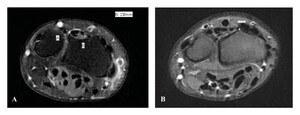
There were 31 images of the right wrist and 28 images of the left wrist. The average age of the patients was 35.8 years old (range: 21-65 years). The average depth of the sulcus was 1.30 ± 0.61 mm (range: 0-3.1) [Figure 2]. The average sulcus depth for females was 1.34 ± 0.60 mm (range: 0-3.1) and 1.30 ± 0.64 mm (range 0-2.8) for males. The sulcus depth measured ≥2 mm in 14% of the wrists studied, and the absence of a sulcus, which equaled 0 mm in depth, was found in 3% of patients [Figure 3A and 3B]. There was no significant difference in sulcus depth between gender (P = 0.8) or wrist laterality (P = 0.2).
The radiocarpal joint averaged 6.1 ± 2.9 mm distal to the sulcus measurement location. The distance of the radiocarpal joint demonstrated no significant difference between gender (P = 0.9) or wrist laterality (P = 0.7). There was also no correlation between the sulcus depth and distance of the radiocarpal joint (R2=0.02).
DISCUSSION
Lister’s tubercle is a prominent anatomical landmark on the dorsal aspect of the radius that creates ulnar and radial margins. These two margins converge to form a dihedral angle ranging from 110-135 degrees.13 While Clement et al. found Lister’s tubercle to average 3.6 mm in height, the depth of the concave sulcus ulnar to the tubercle has yet to be quantified.14 Increased understanding of this concave sulcus, which we have called the “dorsal ulnar blind spot,” may aid in intraoperative evaluation of dorsal screws in volar plating for distal radius fractures. Ulnar to the tubercle, the tendons of extensor pollicus longus (EPL), extensor indicis proprius (EIP), and extensor digitorum communis (EDC) are encountered. Thus, care must be taken when placing the dorsal screws. The third and fourth compartments in our study were contained in a concave sulcus 97% of the time. The remaining 3% of individuals in our study had a flat surface in this region [Figure 3B]. The dorsal ulnar sulcus had a depth ranging from 0 mm to 3.1 mm, demonstrating great variability in this area. Thus, highlighting the importance of knowing the sulcus anatomy and its variability due to its potential to obscure dorsal screw penetration.
Radiographic evaluation of dorsal screw penetration continues to be a debated topic. Our study utilized MRI to evaluate the bony anatomy of the dorsal sulcus. While computed tomography (CT) scans traditionally evaluate bony anatomy, recent studies have shown that MRI is sufficient.15 The height of Lister’s tubercle can obscure visualization on lateral radiographic views, while the depth of the dorsal ulnar sulcus can obscure visualization on oblique lateral views. Because of this unique anatomy, failure to detect dorsal screw penetration using only standard lateral and oblique X-rays remains a possible hindrance in the volar plating of the distal radius. Instead, axial radiographic views have been described to assist in the assessment of screw length, with one example being the skyline view. The skyline view takes axial images of the elbow in 75°-80° flexion and the wrist in maximum volar flexion.15,16 Riddick et al.17 compared the ability of the pronated oblique, lateral, and skyline views to detect screw penetration and found the skyline view to be the most sensitive, specific, and accurate at 83% for each criterion. The pronated oblique view was less accurate at 77%, and the standard lateral radiograph was only 51% accurate.17 Studies have recently attempted to use alternative axial projections of the dorsal distal radius.18,19 These unique fluoroscopic views may have clinical value in evaluating screw penetration. However, their use may be limited in comminuted fractures and polytrauma patients with other hardware in the field.
The distal screws of volar plates are generally locking. Therefore, bicortical fixation is generally unnecessary. However, it is preferable to obtain a screw of suitable length to bolster the subchondral surface of the joint and avoid dorsal collapse. This new understanding of the dorsal sulcus has modified our approach to screw length choice. Intraoperative oblique lateral fluoroscopic images continue to be utilized in part to detect dorsal screw penetration. Though, based on our data regarding the dorsal ulnar sulcus, we now suggest subtracting 2-3 mm from the observed screw length for screws positioned centrally in the sulcus. This technique has been beneficial for fractures with dorsal comminution, wherein depth gauge measurements and axial fluoroscopic images can be indeterminate. Using this new method, we have seen a decline in extensor tendon complications at our institution. Prior to this study, our incidence rate of dorsal tendon irritation was 2% (3/163) and has since been reduced to 0% (0/151). While the difference is not substantially significant (P = 0.25), we are encouraged by the trend.
This study is not without limitations. There is an intrinsic human error in measuring the average dorsal sulcus depth and radiocarpal joint length on each axial cut of the MRI. A single measurement was recorded by both an orthopaedic surgery and radiology team member present for each wrist MRI. However, interobserver reliability was not explicitly measured. Thus, repeating this study using two independent reviewers could address this. While we systematically approached each measurement using Lister’s tubercle and were weary of any exclusion criteria, mentioning this potential for error is important. Additionally, our small sample size limits the power of our study. The dorsal ulnar blind spot is poorly characterized in surrounding literature, making it an opportunity for future studies to expand the sample size and enhance volar plate fixation of distal radius fractures.
CONCLUSION
The dorsal ulnar sulcus remains an important area for surgeons to quantify during volar plate fixation of distal radius fractures. Our study quantified the anatomic variance in this area and allowed us to decrease the incidence of dorsal tendon irritation at our institution to 0%. Overall, increased awareness of the anatomical variation of the dorsal ulnar sulcus or “blind spot” may help surgeons reduce the incidence of extensor tendon complications in patients undergoing volar plate fixation of distal radius fractures.
Declaration of conflict of interest
The authors do NOT have any potential conflicts of interest in the information and production of this manuscript. Dr. Vishal Khatri became a consultant for DePuy Synthes of J&J and Globus Medical years after this study was conceptualized and data collection and analysis was completed.
Declaration of funding
The authors received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of ethical approval for study
This study, #11-150, was approved by our Institutional Review Board on December 31st, 2011, and informed patient consent was subsequently waived due to the retrospective nature of the study.
Declaration of informed consent
There is no information, including names, initials, hospital identification numbers, or photographs, that can be used to identify patients who took part in this study.