INTRODUCTION
Clavicle fractures are common, accounting for 2% to 10% of all fractures sustained, depending on the age group, as well as up to 44% of shoulder girdle fractures.1 Approximately 1 in 1000 people sustain a clavicle fracture every year.2 Historically, studies have shown that clavicle nonunion rates for conservative treatment are relatively low, typically under 1%.3,4 However, more recent prospective studies on the nonoperative management of displaced midshaft clavicle fractures in adults have reported nonunion rates ranging from 13% to 20%, associated with risk factors such as increased displacement, comminution, and smoking.5 Additionally, these studies indicate an 18-33% reduction in shoulder muscle strength, poor early shoulder function, and residual issues in up to 42% of patients six months post-injury.6–8
Growing awareness of the suboptimal outcomes associated with nonoperative treatment has led to a rise in the popularity of primary surgical fixation for these fractures. A 2012 meta-analysis of 6 randomized controlled trials (RCTs) by Mckee et al. found lower complication and nonunion rates and earlier return to function with surgical intervention compared to nonoperative management.9 Given that clavicle fractures often affect the young and active demographic, achieving a rapid return to function and early bone healing is a priority. This goes with traditional goals like restoring shoulder range of motion and strength and preventing long-term complications such as nonunion and symptomatic malunion.
The benefits of surgery in young, active populations have been suggested.10 However, there is a paucity of literature on treatment trends organized by demographic data, especially sex and race. A 2017 study on data from 2005-2010 showed associations between surgical intervention rates and varying socioeconomic factors, including race, insurance, and income level, with white race, private insurance utilization, and higher income being positive predictors.11
This study used large population-level data to examine trends in the number of clavicle fractures undergoing open reduction internal fixation (ORIF). The secondary aim was to elucidate demographic factors associated with ORIF, including race, ethnicity, and sex. With the advent of deidentified patient databases like TriNetX, large-scale analysis is now possible. Due to the increased sample size, this type of study is ideal to spot trends that may not have been possible when querying individual healthcare systems or statewide databases.
As surgeons continue to adopt evidence-based medicine, recent literature supporting surgical intervention for clavicle fractures has risen. Additionally, known demographic disparities may be at play. It was hypothesized that there was an overall increase in the rate of ORIF for clavicle fractures during the study period and that there were significant associations between demographic factors and rates of surgical intervention.
METHODS
Data Sources
In November 2024, the TriNetX US Collaborative Network was queried, which provided access to electronic medical records from approximately 113 million patients in the United States from 67 healthcare organizations. This network was chosen since it contains the broadest population group within TriNetX available for analysis exclusively within the United States.
The TriNetX database does not involve identifiable patient information and is subsequently exempt from Institutional Review Board review and approval. All Healthcare Organizations (HCOs) within the network follow a deidentification process conforming to Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule standards. Information includes patient demographics such as age, sex, ethnicity, and race. Data includes diagnosis codes (International Classification of Disease Version 10 Clinical Modification, ICD-10-CM) and procedure codes (Current Procedure Terminology, CPT).
Patients
The TriNetX US Collaborative Network was queried for patients aged 0-90 diagnosed with a closed displaced midshaft clavicle fracture from January 1st, 2017, to December 31st, 2022 (n = 68,301 patients). ICD-10-CM codes (S42.021A, S42.022A, and S42.023A) were used to identify this group. This cohort was then classified into the ORIF or nonsurgical groups by querying the population using CPT code 23515. [Table 1] All patients who received CPT code 23515 within 90 days of the clavicle fracture were included in the ORIF group. All patients who did not have the CPT code 23515 comprised the nonsurgical group. Age groups were stratified to represent childhood (0-17 years), early adulthood (18-39 years), middle adulthood (40-64 years), and late adulthood (65-90 years) populations.
Exclusion criteria included patients who had already been diagnosed with a clavicle fracture before the study period and those who had previously undergone clavicle ORIF before the study period. This was a cumulative criterion, meaning that an individual diagnosed with a clavicle fracture in 2017 would not be counted again if diagnosed with a clavicle fracture in 2022. Patients with missing demographic information were also excluded from the analysis.
Intervention and Statistical Analysis
The primary outcome was the rate of clavicle fractures treated with ORIF. Other variables analyzed included age, sex, race, and ethnicity. ORIF trends over time were analyzed using the Cochran-Armitage Test, with P < 0.05 selected as significant. Odds ratios (OR) and 95% confidence intervals (CI) were calculated to determine the rates of surgical intervention among the different demographics, with P < 0.05 selected as significant.
RESULTS
From 2017 to 2022, 68,301 patients were diagnosed with displaced midshaft clavicle fractures according to the criteria. Of those with known sex, males were more likely to sustain this fracture, accounting for 70% of patients. Of those with known ethnicity, 18% were Hispanic or Latino, while 82% were non-Hispanic. White race was the most common, accounting for 86.8% of individuals studied. There was a unimodal age distribution with a peak in young adulthood and a slight taper in the aging populations. The least represented age group was 65-90 years, accounting for 15% of the cohort.
Among all patients, 14% were treated with ORIF (n = 9711/68301). An overall increase in the rate of ORIF was observed for clavicle fractures from 13% in 2017 to 15% in 2022 (P < 0.001) [Table 2].
A significant increase in ORIF rates was observed for age groups 0-17 years (0.4% to 2.7%, P < 0.001), 18-39 years (13.4% to 26.8%, P < 0.001), and 40-64 years (19.3% to 25%, P < 0.001). The late adulthood age group (65-90 years) was observed to have a decrease in ORIF rates from 10.5% to 8.5%; however, this was not significant [Figure 1].
Individuals aged 18-39 years showed a significantly higher association of undergoing operative intervention compared to individuals aged 0-17 years (OR 18.41, 95% CI 16.24-20.85) and individuals aged 65-90 years (OR 2.24, 95% CI 2.08-2.41). However, they were less associated with operative intervention than individuals aged 40-64 (OR 0.86, 95% CI 0.81-0.90). Additionally, individuals aged 40-64 were more associated with operative intervention than those aged 65-90 (OR 2.61, 95% CI 2.42-2.82). [Table 3]
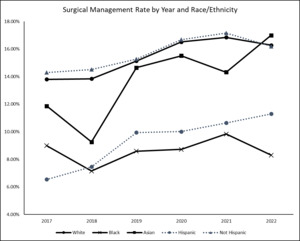
A significant increase in ORIF rates was observed for Whites (13.8% to 16.3%, P < 0.001), Asians (11.9% to 17%, P < 0.01), Hispanics (6.6% to 11.3%, P < 0.001), and non-Hispanics (14.3% to 16.2%, P < 0.001). A decrease in ORIF rates was observed for Blacks from 9% to 8.3%; however, this was not significant. [Figure 2]
Males exhibited a higher association with ORIF than females (OR 1.49, 95% CI 1.42-1.57). Whites were more associated with surgical treatment than Blacks (OR 1.85, 95% CI 1.67-2.06), American Indian/Alaska Natives (OR 2.22, 95% CI 1.53-3.22), and Native Hawaiian/Pacific Islanders (OR 2.01, 95% CI 1.47-2.77). There was no significant difference in surgical management rates between Whites and Asians. Non-Hispanic/Latino individuals were more associated with undergoing surgery than those of Hispanic or Latino ethnicity (OR 1.66, 95% CI 1.55-1.78). [Table 3]
DISCUSSION
This study provides insight into the trends and demographic factors associated with ORIF of midshaft clavicle fractures. The hypothesis of this study was supported, with the overall rate of surgical management significantly increasing from 2017-2022. Furthermore, various demographic factors were associated with increased odds of surgical management. Non-Hispanic men were more associated with ORIF overall. Additionally, Whites and Asians were more associated with surgical management than Black, Native, and Pacific Islander Americans.
The overall increase of ORIF rates from 2017 to 2022 demonstrates a shift towards more aggressive management of these fractures. The most significant increases in incidence of operative management were found in the younger age groups (0-17 years and 18-39 years). Additionally, significant differences were found between the rates of ORIF for males and females as well as between races. The findings in this study suggest that there are associations between certain demographic groups and surgical intervention, highlighting patterns in treatment that could provide greater awareness of care.
Historically, closed midshaft clavicle fractures have been treated conservatively, barring only the most severely displaced fractures. More recent literature suggests that this previously accepted practice leads to decreased functional outcomes and increased rates of malunion and nonunion.10,12 The findings in this study suggest that surgeons are shifting their practice to align with recent literature. Fanter et al. indicated that increased activity levels and athletics could play a role in operative management of adolescents, with better outcomes and a more rapid return to sport than conservative management in borderline or displaced cases.13 Multiple studies, including a 2022 meta-analysis by Yan et al., found that surgical intervention is associated with significantly better long-term outcomes with higher functional scores and lower rates of malunion.9,10,14 Younger adults would benefit the most from long-term functional outcomes given their increased post-operative lifespan, which could play a role in the decision to manage these types of fractures operatively. Furthermore, those in this age group may desire a more rapid return to functionality as they are more likely to be working or child-rearing.
Interestingly, this study found that individuals aged 18-39 were slightly less associated with surgical intervention than those aged 40-64. This appears to be at odds with literature demonstrating that younger adults are more likely to undergo fixation of these fractures than older adults.15,16 Sepheri et al. looked at age groups 18-30, 30-50, and greater than 50 in a Canadian population, while Yang et al. only examined US adults above and below 65. The findings of this study could point to a difference in management between US and Canadian surgeons for these groups, suggesting a bias towards operatively treating slightly older patients in the US. Furthermore, without additional stratification of age groups, it is difficult to know if the younger portion of the 18-39 age group with potentially lower surgical intervention rates is skewing the entire cohort. Another explanation for this finding could be the lower health insurance rate among younger individuals. Individuals in the 18-39 age group have lower rates of health insurance coverage than those aged 40-64, according to a US Census report.17 While being uninsured may not stop an individual from coming into an emergency department or urgent care to treat an acute clavicle fracture, it could be a reason for one to forgo expensive surgery. Furthermore, Figure 1 suggests that after 2021, the difference in operative rates between these age groups may diminish.
Males were also much more associated with operative management than females. There is a lack of quality research addressing this fact. However, a 2022 epidemiological study of 2422 clavicle fractures by Kihlström et al. found that males were more likely to sustain clavicle fractures from transport accidents such as motorcycle or bicycle crashes, while females were more likely to sustain fractures from a fall.17 This suggests that the discrepancy in operative management could be due to fracture severity or poly-trauma. High-energy injuries associated with activities more commonly performed by males could explain the higher surgery rates in this cohort compared to low-energy falls associated with females. Additionally, scar cosmesis is of great importance in the decision to pursue operative management. This is elaborated by Lari et al., who found that females greatly favored scar cosmesis over males.18 Thus, a surgical scar on an exposed area like the collarbone may account for decreased female operative management. Although the above-mentioned factors could play a role in the discrepancy in ORIF rates between males and females, surgeons should strive to deliver evidence-based treatment while balancing the patient’s preferences.
There were significant differences in operative rates between racial and ethnic groups. Black and Native Americans/Pacific Islanders were far less associated with ORIF than any other racial group by a large margin. This finding is in support of prior research showing Black race is associated with lower rates of surgical intervention for clavicle fracture, as well as orthopaedic traumas in general.11,18,19 Interestingly, this study found no difference in the rate of surgical management between Asians and Whites. There is minimal research exploring this fact. However, Schairer et al. did another study that stratified clavicle fracture surgical management by race and found that Asians were less likely to be managed surgically than Whites.11 That study, however, only looked at patients from Florida and California, which may not represent the US as a whole. Furthermore, a 2018 meta-analysis of racial disparities in surgical care in the United States found that many studies disagreed regarding the treatment of Asians in comparison to Whites, with some finding care discrepancies while others finding parity.20 It was suggested that this is due to the innately incorrect classification of Asians into a single race, as, in reality, this group is made up of many backgrounds with vastly different socioeconomic status and healthcare literacy.21 This challenges prior orthopaedic literature demonstrating that non-white race, including Asian race, was associated with lower rates of operative management of orthopaedic trauma and hip fractures. However, the findings in this study regarding other races support these claims.18,22
While drawing conclusions regarding Native Americans is difficult due to the small sample size, the significant disparity in ORIF rates for Blacks raises important questions about the underlying cause of these discrepancies. Differential utilization of healthcare resources has been well documented within the field of orthopaedics. Arthroplasty utilization, spinal arthrodesis, and fracture care are notable examples where socioeconomic factors play a role in management decisions.22–24 A 2016 study by Katz explores total joint arthroplasty (TJA) and possible causes of the disparity in utilization, including trust in providers, referral patterns, and patient understanding/education about a procedure.25 This reinforces the understanding that there may be differences in healthcare-seeking behavior among the Black population, possibly stemming from cultural factors or mistrust of the healthcare system.
Furthermore, Hispanic individuals were far less associated with ORIF compared to non-Hispanics. This finding is well documented in prior literature, which demonstrates that minority ethnic groups are less likely to undergo surgical intervention across multiple specialties, including cardiothoracic, orthopedic, and colorectal surgeries.26 One underlying cause of this disparity could be explained by the findings of Escobedo et al., who examined barriers to healthcare for Latinos in the United States. They found that among Hispanics, the rate of limited English proficiency (LEP) is significantly higher than in other racial or ethnic groups. This was a large self-reported barrier to healthcare access.27 It is reasonable to assume that this finding also applies to the surgical treatment of clavicle fractures. This could result in Hispanic patients being less likely to follow up for surgery after an initial visit for a fracture, resulting in lower ORIF rates for this population.
While this study can shed light on the differences in operative management of clavicle fractures between different demographic groups, it is unable to specifically define the underlying reasons for these differences. Future research should include prospective studies exploring the underlying factors driving the disparity between groups, including insurance coverage, socioeconomic/employment status, child-rearing responsibility, and cultural differences. Furthermore, the method of surgical management should be explored, comparing outcomes of newer intramedullary or minimally invasive plate osteosynthesis (MIPO) to traditional ORIF.
This database study, while large in scale and scope, has limitations. The retrospective nature of the data and lack of detail about the clavicle fractures sustained, including location, displacement, and co-occurrence with other traumatic injuries, may limit the generalizability of these findings. For instance, common indications for surgical intervention in closed clavicle fracture cases, such as neurovascular injury, skin tenting, and gross deformity, cannot be accurately assessed. Additionally, multivariable analysis and controlling for confounding comorbidities would strengthen these conclusions and establish a causal relationship. Also, since the database queried relies on administrative-level information, this study is only as accurate as the administrative data added for each patient. Specifically, not all patients had all demographic information included and were thus excluded from the analysis. This introduces selection bias as specific demographic groups are more likely to miss this information than others. As TriNetX is an active database, it is continuously being updated, meaning that throughout the data collection period, numbers could have shifted, affecting the overall results.
CONCLUSION
Operative fixation of closed midshaft clavicle fractures has risen significantly from 2017 to 2022. Adolescents and young adults saw the largest increases in operative management rates during this period. Different rates of surgical intervention were apparent among various demographics, with males more associated than females with ORIF and minority groups less associated with surgical management than non-Hispanic Whites. These discrepancies must be addressed by raising awareness of implicit biases among providers, improving access to orthopaedic care among underserved communities, and future research focused on the root cause of these disparities.
Declaration of conflict of interest
The authors do NOT have any potential conflicts of interest for this manuscript.
Declaration of funding
The authors received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of ethical approval for study
This study did not require ethical approval from an Institutional Review Board (IRB) as it utilized de-identified and anonymized data, which do not meet the criteria for human subjects research under applicable regulations.
Declaration of informed consent
There is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify patients.