INTRODUCTION
It has been estimated that proximal humerus fractures account for 5-6% of all fractures.1 With our population growing and living longer, a 28% increase in the population-adjusted incidence of proximal humerus fractures has been noted in patients aged 65 years or older from 1990 to 2010.2 Although most proximal humerus fractures are treated nonoperatively, open reduction internal fixation (ORIF) with plate fixation is the most common operative treatment, followed by reverse total shoulder arthroplasty.1 Other surgical treatment options for proximal humerus fractures include percutaneous pinning, intramedullary nailing, and hemiarthroplasty. Moreover, with the advent of peri-articular anatomic locking plates, recent studies have demonstrated an increasing trend toward proximal humerus fracture fixation.1,2
Despite increasing utilization of proximal humerus fracture fixation with locking plates, challenges with this technique include screw penetration, varus collapse, nonunion, and malunion.3,4 Moreover, the estimated risk of avascular necrosis after ORIF of a proximal humerus fracture has been reported to range from 0% to 15%.5 Although the optimal surgical treatment with either fracture fixation versus arthroplasty for proximal humerus fractures remains controversial, recent studies have reported good functional outcomes with locking plate fixation.6,7 Biomechanical studies have also described locking plate fixation as a reliable construct.8 This review aims to provide an overview of the surgical technique using locking plate fixation for the treatment of proximal humerus fractures.
INDICATIONS & CONTRAINDICATIONS
While approximately 80% of proximal humerus fractures can be successfully treated non-operatively, there remain a variety of cases than may benefit from locking plate fixation. Although absolute indications for surgical intervention are limited and debatable, they may include fractures of the proximal humerus with an associated glenohumeral joint dislocation, open fractures, and a fracture associated with neurovascular injury.
Age is an important determinant for fracture management with proximal humerus fractures. Younger and active patients with displaced and/or multi-part fractures are indicated for locking plate fixation. In contrast, older patients, even in the setting of displacement, are often treated with non-operative management. However, there is evidence that activity level and social independence in older patients correlate with functional outcomes, and these factors should also be considered in determining the best treatment course.9 Regarding injury morphology, relative indications for ORIF include displacement of the humeral head from the shaft, 5mm or more displacement of the tuberosities, varus or valgus angulation of 30 degrees or more, fracture-dislocations with retained soft tissue attachments to the humeral head, and displaced humeral head marginal articular fractures with 2mm or more of displacement.5
Contraindications for proximal humerus fracture locking plate fixation include patients with severe comorbidities, fractures thought to be irreparable, and fractures with severely compromised blood supply to the humeral head such as those with a head-splitting component, extensive impaction or comminution of the articular surface, or fracture-dislocations with loss of soft tissue attachments to the humeral head.5 Although debatable, these fracture types may be more amenable to arthroplasty compared to locking plate fixation.
SURGICAL TECHNIQUE
Surgical Preparation
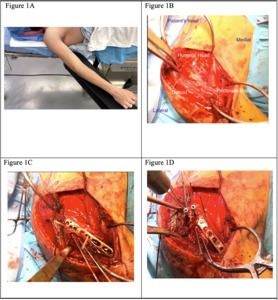
The authors’ preferred method of patient positioning for proximal humerus fixation is supine. The arm is abducted about 45 degrees on an arm board, allowing the surgeon and assistant to stand on either side of the operative arm [Figure 1A]. This also allows for the C-arm image intensifier to come in from the contralateral side to allow easy access to the surgical field. Alternatively, the patient may be positioned in the beach chair position.
Surgical Equipment
Necessary surgical equipment for proximal humerus locking plate fixation includes power drills, an anatomic proximal locking plate with corresponding screws, Kirschner wires, and non-absorbable heavy sutures. Self-retaining (i.e., Gelpy retractors) or large reverse retractors (i.e., Hohmann retractors) may also aid in retraction during the approach and fixation. C-arm fluoroscopy should also be available during the procedure.
Superficial Exposure
The authors’ preferred approach is the deltopectoral interval. The coracoid, acromion, AC joint, and deltoid insertion are identified. The planned deltopectoral incision is marked slightly more lateral from coracoid distal to deltoid insertion. This allows easier access to the lateral aspect of the proximal humerus, where the plate will be applied. A scalpel is used for sharp dissection down to the subcutaneous tissue. Next, dissection proceeds to the level of the deltoid fascia using dissecting scissors and augmented with the use of cautery as needed to control bleeding and maintain hemostasis with care taken to stay above the fascia. Once at the level of the deltoid fascia, the cephalic vein should be readily identified and will guide the deltopectoral interval. The cephalic vein can be mobilized medially or laterally, and its branches can be cauterized as needed to aid in mobilization. Blunt dissection can then be used to widen the deltopectoral interval. Retractors are placed, but additional deltoid release may be necessary to achieve full exposure extending to the level of the acromion proximally [Figure 1B].
Deep Exposure
Once the humerus is exposed, the biceps tendon, the pectoralis insertion, the latissimus insertion, tuberosities, and the rotator cuff are identified. The fracture site is examined, and displaced fragments, including tuberosities in a multi-part fracture, can be tagged with heavy sutures such as #5 ethibond to aid in identifying and mobilizing fragments. Sutures can also be used to repair tuberosities to each other or to the plate later.
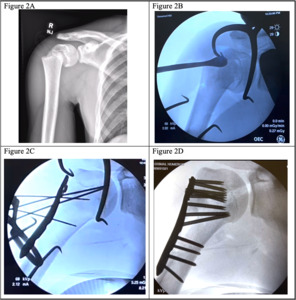
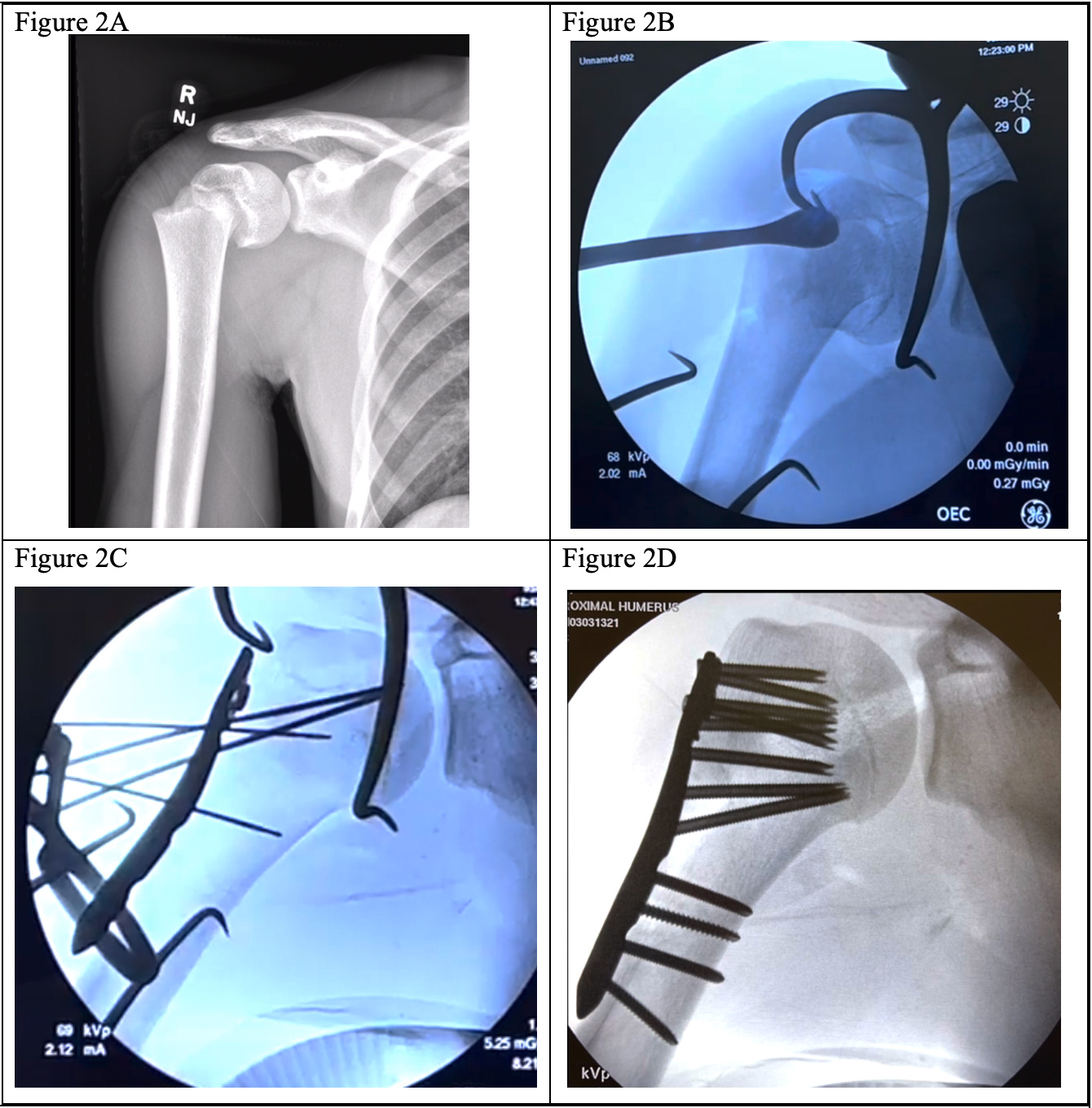
A cobb elevator can then be placed within the fracture site to elevate the humeral head relative to the shaft. In contrast, the retention suture in the humeral head is tensioned to provide valgus stress [Figure 2B]. This maneuver can assist in correcting the varus collapse of the fracture. Once reduced, the fracture can be provisionally fixed with Kirschner wires [Figure 1C]. Alternatively, the plate can be applied to the distal shaft, and the proximal, reduced head can be pinned to the plate. The proximal end of the proximal humerus locking plate is preloaded with heavy sutures to augment the repair by placing sutures through the rotator cuff and any displaced tuberosity fragments post-fixation.
Fixation
The following technique is associated with figures utilizing the proximal humerus anatomic locking plate system manufactured by DePuy Synthes (LCP Proximal Humerus Plate, DePuy Synthes, West Chester, PA). An anatomic locking plate is applied to the lateral aspect of the humerus just lateral to the biceps tendon, medial to the deltoid insertion distally, held in place with Kirschner wires proximally and distally, and alignment is confirmed using C arm fluoroscopy [Figure 2C]. Proper plate positioning is important to prevent functional limitations or damage to surrounding structures. Therefore, the plate should be positioned inferior to the superior aspect of the greater tuberosity and posterolateral to the bicipital groove to prevent shoulder impingement or injury to the biceps tendon, respectively.5
Initial fixation begins with cortical screws in the shaft. Once two points of fixation have been secured in the shaft distally, attention is then turned to the head proximally. If the locking plate has screw guides, a guidewire can be used over which cannulated locking screws can be placed across the plate into the head [Figure 1D].
Initial screws placed in the proximal humeral head can be non-locking conical screws that allow compression of the humeral head to the plate and further minimize residual varus alignment. The remaining proximal screws are placed locking until the humeral head is filled with screws. Care must be taken to avoid violation of the articular surface. Final distal shaft screws are then placed as desired in either a locking or non-locking fashion. If preferred, the most proximal conical screws can also be switched to a locking screw. The final calcar screw is placed with the goal of placing as close to the inferior aspect of the head as possible to maximize construct stability and mitigate the risk of varus collapse of the humeral head. In a patient with open growth plates, proximal screws are left intentionally short to preserve the integrity of the physis [Figure 2D]. In skeletally mature patients, the goal is to achieve an appropriate screw length that will capture subchondral bone.
Rotator Cuff Repair and Wound Closure
Preloaded sutures are used to repair the rotator cuff to the proximal humerus and plate to minimize varus collapse. This is especially helpful in older patients in whom the risk of varus collapse may be higher. In multi-part fractures, each part can be repaired to the plate using retention sutures to help construct stability and rigidity. The wound is irrigated and closed in a layered fashion, including the subcutaneous tissue and skin only. Care is taken to avoid placing sutures in the deltopectoral interval.
Post-operative Management
Patients are placed in a sling for 1-2 weeks postoperatively, after which they may begin formal physical therapy. In the immediate postoperative period, patients are allowed to use their arms for activities of daily living as tolerated.
DISCUSSION
Although the optimal surgical treatment of proximal humerus fractures remains controversial, recent reports have demonstrated that locking plate fixation is a reliable fixation method.6 However, this surgical method is not without complications, including screw penetration, avascular necrosis, malreduction, hardware failure, and nonunions.3 In addition to the pearls described, previous studies have also reported the importance of obtaining medial column support with an inferiorly placed calcar screw, avoiding lateralization with distal plate fixation, and possibly increasing the number of screws in the humeral head with shorter lengths to reduce the risk of screw penetration.4,10
Despite the lack of consensus regarding nonoperative compared to operative treatment of proximal humerus fractures, prior studies have described improved outcomes with regard to pain and function with surgical management.6,7 Furthermore, Robinson et al. reported an estimated 74% survivorship of primary ORIF until any reoperation, demonstrating that proximal locking plate fixation can be a reliable option in the appropriately selected surgical candidate.7
Limitations with this surgical technique include possible increased difficulty with greater tuberosity fracture reductions when using the deltopectoral approach compared to the deltoid splitting approach. Additionally, using a pneumatic arm holder may improve appropriate arm position and visualization without needing another surgical assistant. Furthermore, grafting or bone cement options may need to be utilized with more comminuted or impacted fractures with a large portion of bone missing once reduced. Future studies assessing optimal patient indications and clinical outcomes of augmentation are needed further to understand the best management of these complex fractures. In addition, clinical studies of locking plate fixation with variable angles and anatomic plates that include the tuberosities may further our understanding of the most favorable fixation for various fractures.