Introduction
The humeral shaft fracture nonunion rate after open reduction internal fixation (ORIF) is 4-10%.1 Known nonunion risk factors include mechanical instability, inadequate vascular supply, poor bone-to-bone contact, and metabolic or endocrine factors. The latter includes infection, systemic medical conditions (such as diabetes mellitus), nicotine or radiation, alcohol abuse, vitamin deficiencies, and malnutrition.2,3 A recent multicenter analysis of the association between multiple medications and fracture nonunion found only bisphosphonates and vascular nonunion to be associated,4 but this analysis did not include any human immunodeficiency virus (HIV) pre-exposure prophylaxis (PrEP) medications.
HIV PrEP is increasing worldwide, with approximately 250,000 people in the United States prescribed PrEP in 2020.5 Currently, there are two common oral formulations of PrEP: (1) emtricitabine and tenofovir disoproxil fumarate (FTC-TDF) and the prodrug (2) emtricitabine and tenofovir alafenamide (FTC-TAF). There is limited evidence on the interaction between these drugs and bone health. In the initial study cohort of 1,251 patients on FTC-TDF, only 1% reported bone fractures, and no nonunions were documented.6 Additional studies have found incremental differences in bone mineral density (BMD) and renal function but no differences in clinically meaningful adverse events.7–10
Here we report a case of a healthy, young male patient with a humeral shaft fracture that resulted in a nonunion after ORIF while on FTC-TAF.
Case Report
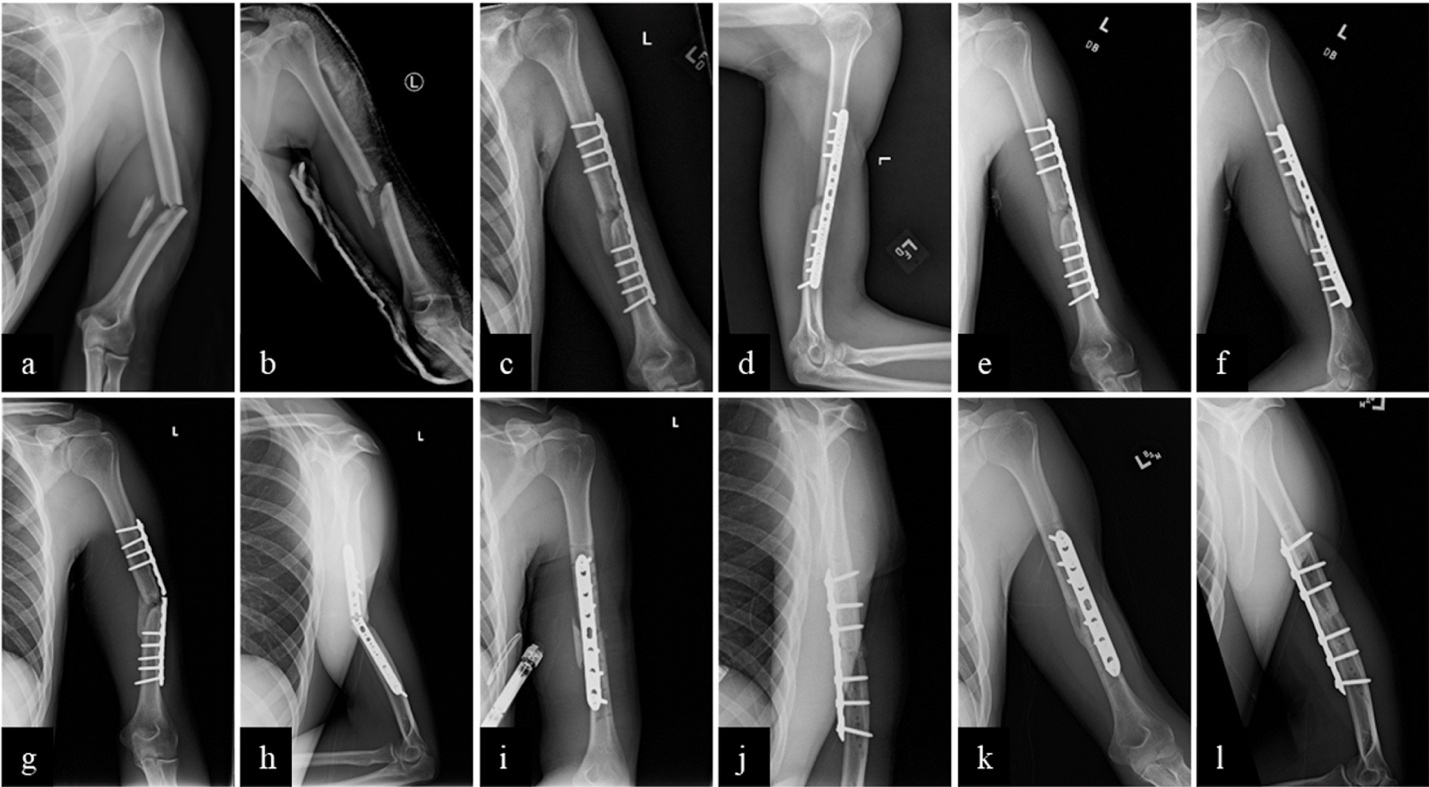
Patient Information: A 24-year-old, right-hand-dominant healthy male patient with a history of taking FTC-TAF HIV prophylaxis presented to the emergency department on the day of injury with left arm pain and deformity after a fall approximately 15 feet through a skylight. Injury radiographs showed a displaced, comminuted closed midshaft left humerus fracture [Figure 2a, b]. He was neurovascularly intact. Social history was significant for being a current medical student and a nonsmoker with no considerable alcohol intake. His only medication and medical history were taking FTC-TAF HIV PrEP for three years. He had no medical or surgical history or family history of metabolic or bone disorders. The patient was treated with a provisional coaptation splint. On post-injury day four, the patient underwent outpatient left humerus ORIF. Standard cefazolin surgical prophylactic antibiotics were administered. ORIF was performed with a 14-hole large fragment lateral locking plate [Figure 2c, d]. The patient underwent an initially uneventful postoperative course [Figure 2e, f]. At 11 months post-op, the patient re-presented for an atraumatic increase in left arm pain.
Clinical Findings: There was no tenderness to palpation at the 3-month and 6-month follow-ups from the index procedure. On re-presentation at the 11-month follow-up, he remained neurovascularly intact but had new onset left arm tenderness.
Timeline: [Figure 1]
Diagnostic Assessment: Eleven-month post-operative radiographs demonstrated humerus shaft nonunion and lateral plate fatigue fracture with varus alignment [Figure 2g, h].
Therapeutic Intervention: The patient underwent revision ORIF via lateral approach with hardware removal, nonunion debridement, and anterior 4.5 compression plate application [Figure 2i, j]. Standard cefazolin surgical prophylactic antibiotics were administered. Intra-operatively there was a medial bridging callus, persistent mid-section humerus fracture line, and plate fatigue fracture. Intraoperative cultures were negative. Post-operatively, weight bearing was limited to three pounds, and FTC-TAF was held for two months and confirmed by the patient report.
Outcomes: Radiographs at 6-week, 3-month, and 6-month follow-ups demonstrated interval callus formation, and the patient reported improved left arm pain and function [Figure 2k, l].
Discussion
Here we present the case of nonunion after a comminuted high-energy humeral shaft fracture. Mechanical nonunion must first be considered. The presence of bridging callus intraoperatively during revision ORIF suggests adequate fracture stability for healing. Alternatively, too stiff of fixation could also inhibit fracture healing, as has been described in femur fracture lateral plating by Lujan et al.11 Though we cannot definitively exclude mechanical nonunion, other risk factors for nonunion must also be considered. Brinker et al. reported that 84% of nonunions in fractures with adequate stabilization and bone-to-bone contact underwent an endocrine and metabolic workup and were diagnosed with a new metabolic or endocrine abnormality, most commonly vitamin D deficiency in 57% of patients.12 In contrast, a recent multicenter cohort study by Shapiro et al. found that serologic abnormalities are less common than previously reported by Brinker et al.4,12 Instead, they found smoking, alcohol abuse, and diabetes mellitus as three significant modifiable risk factors associated with nonunion. They reported that a complete metabolic workup for all nonunion patients was not cost-effective.4 In agreement with this,4 we did not pursue a complete metabolic and endocrine workup to exclude other causes of nonunion. Thus, this case report is limited as we cannot exclude other potential abnormalities, such as undiagnosed vitamin D deficiency.
Our patient experienced nonunion while taking HIV PrEP and subsequently developed radiographic and clinical evidence of fracture healing when FTC-TAF PrEP was held for two months post-revision ORIF. Without other identifiable nonunion causes, this suggests FTC-TAF may be associated with nonunion. A recent review article9 on tenofovir reported that BMD decreases when antiretroviral therapies start, particularly with tenofovir. Multiple proposed mechanisms exist for how tenofovir formulations (TDF and its prodrug TAF) impact bones.9 In vitro studies suggest tenofovir directly interacts with genes involved in osteoclasts and osteoblasts cell signaling, energy, and amino acid metabolism. Alternatively, tenofovir may interfere with renal proximal tubule secretion to indirectly interfere with vitamin D metabolism.9 Though the exact mechanism is unclear, this translates to a decrease in BMD of approximately 1-3% greater in patients taking TDF versus non-TDF-containing antiretroviral regimens.7,9,13–15 BMD decrease is lower in patients taking the TAF prodrug than TDF.7 BMD decreases in the first 48 weeks of treatment initiation but was not progressive with continued therapy.16 One study reported that decreased BMD could be mitigated by vitamin D and calcium supplementation over the first 48 weeks of therapy.8 The clinical implication of this decreased BMD is not clearly defined in the literature, but literature on osteoporotic fragility fractures consistently demonstrates an inverse relationship between BMD and fragility fracture risk.17 One study reported an increased risk of fragility fractures with tenofovir,18 while other studies report no difference in fracture risk.9,14,19 To our knowledge, there is no prior literature on the interaction of tenofovir and nonunion.
Here we present a case where FTC-TAF for HIV PrEP might contribute to an increased nonunion risk in an otherwise healthy patient. Though the generalizability of this report is limited, we aim to highlight an important area for future research, given the increased utilization of PrEP medications. Additional sufficiently powered studies are needed to understand the association between HIV PrEP and fracture nonunion.
Declaration of conflict of interest
The author(s) do NOT have any potential conflicts of interest for this manuscript.
Declaration of funding
The author(s) received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of ethical approval for study
Institutional Review Board approval was received from the Thomas Jefferson University.
Declaration of informed consent
There is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify any patients. The patient was informed that data from his case would be submitted for publication and provided consent.
Acknowledgments
n/a.