INTRODUCTION
Necrotizing fasciitis was first described by Hippocrates in the 5th century B.C.E as “erysipelas all over the body when the exciting cause was a trivial accident or a very small wound … erysipelas would quickly spread widely in all directions. Flesh, sinews, and bones fell away in large quantities”.1 Moreover, he commented on the morbidity and mortality associated with necrotizing fasciitis by continuing that: “There were many deaths. The course of the disease was the same to whatever part of the body it spread. Many lost the arm and the entire forearm”.1 Over the years, many terms such as “necrotizing erysipelas,” “streptococcal gangrene,” “suppurative fasciitis,” and “gas gangrene” have been used to describe necrotizing fasciitis.2 The term necrotizing fasciitis was initially coined by Dr. B. Wilson in 1952.3 Recently, the term necrotizing soft tissue infection (NSTI) has been used to encompass all forms of the disease process as they involve a similar diagnostic approach and treatment modalities.2 These infections typically begin in the dermis and the epidermis, commonly spreading to deeper layers and structures such as adipose tissue, fascia, muscle, and connective tissues.3 It is important to note that mortality positively correlates with the initial infection’s depth.2 Often, the disease progresses below the cutaneous structures producing minimal superficial manifestations, making diagnosis difficult.3 Necrotizing fasciitis is a rapidly progressing skin and soft tissue infection (SSTI) that poses a significant threat to life and limb if not diagnosed and treated early.2
Necrotizing fasciitis incidence is estimated at 500 – 1,000 cases per annum, with a reported global prevalence of 0.40 per 100,000. The disease has a 3:1 male-to-female distribution and is more prevalent in men 50 and older.4 Upper extremity infections represent approximately 10-38% of necrotizing fasciitis.5–8 Mortality estimates range from 8.7% to 76%, though without treatment, that number rises to about 100%.4
Recent literature delineates four subtypes of necrotizing fasciitis: Type I synergistic necrotizing fasciitis results from the effects of aerobes, anaerobes, and facultative anaerobes. Type II necrotizing fasciitis is generally monomicrobial, most commonly associated with Group A Streptococcus (GAS) or Staphylococcus aureus, and is the second most common. Gram-negative bacteria cause type III, typically Vibrio spp. or other marine-related organisms, most commonly seen in Asia. Type IV is fungal and is associated with trauma; it is the most aggressive and has a nearly 50% mortality rate.4,9
Through this review, we sought to accomplish two goals: 1) analyze and synthesize the published case reports on upper extremity necrotizing fasciitis and 2) identify any trends in the diagnosis and treatment of upper extremity necrotizing fasciitis.
METHODS
Review Strategy
We sought to identify all published case studies of upper extremity necrotizing fasciitis. Scopus, PubMed, and Medline were systematically searched for papers utilizing the search terms appropriate for necrotizing fasciitis infections of the hand, wrist, and forearms. The terms used were “necrotizing fasciitis,” “hand,” “forearm,” “arm,” and “upper extremity.” Further review was conducted manually from reference lists of identified papers and previous reviews. Limitations were not placed on date or location.
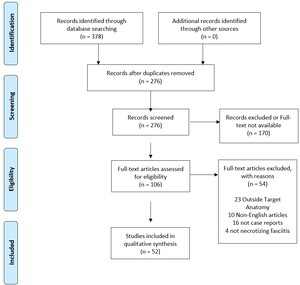
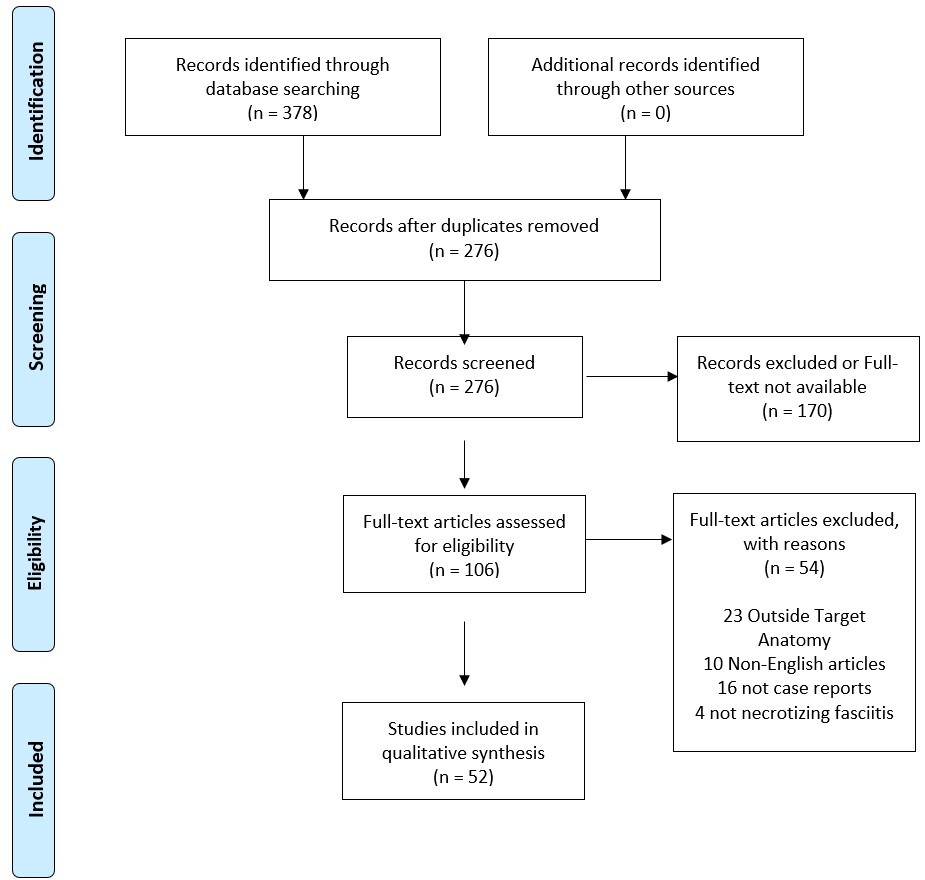
The review for this publication was conducted per PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [Figure 1]. All search results were reviewed by two authors, KD and VB. Initial search results were screened to identify and remove duplicates. Journal articles were read in full and then screened for relevance and included or excluded per criteria. Finally, full-text articles were assessed for final eligibility.
Eligibility
Studies were included in the analysis based on the following eligibility criteria: (1) single case or limited case series, (2) established diagnosis of necrotizing fasciitis in the hand, wrist, or forearm, and (3) English language publication. Studies were excluded if they presented a general review of necrotizing fasciitis, addressed a different diagnosis or necrotizing fasciitis at a different anatomical location, or were unavailable in English.
RESULTS
Patient
Initial database search results identified 378 case reports. Following PRISMA guideline case report exclusion, 52 published case reports of upper extremity necrotizing fasciitis since 1987 were identified, with 54 total patients [Table 1]. Of these, 31 (57%) were male, with a mean age of 56.15 (SD = 20.41, range 1-86). A plurality (30%) of these patients were from the United States of America, with the following common locations being Taiwan (11%), the United Kingdom (UK) (9.3%), and Singapore (9.3%).
Comorbid Conditions
Current case literature suggests local injury is frequently associated with upper extremity necrotizing fasciitis. Most patients in this review (38, 70%) presented with an inciting injury. Many of these injuries (23, 43%) presented independent of other associated comorbidities and consisted of 1 abrasion, one crush injury, one fall, one fracture, ten lacerations, and nine puncture wounds.5,10–31 Traumatic injuries, including penetrating traumas, ulcers, and surgical incisions, are associated with type IV necrotizing fasciitis and subsequent complications, including amputations and death.2,4–6,9,32 A minority of patients had other associated comorbidities independent of injury [Table 2]. Diabetes Mellitus, known to affect microvascular circulation, was the only predisposing condition for necrotizing fasciitis in 4 patients (7.4%).33–36 There were three patients (5.6%)37–39 who presented solely with immunosuppression, most associated with type I necrotizing fasciitis.40–50 Intravenous drug use (IVDU) is related to methicillin-resistant Staphylococcus aureus (MRSA) infections, abscess formation, and type II necrotizing fasciitis, particularly in the upper extremity.2,4–7,9,50 There was 1 (1.9%) person who injected drugs who had no other contributory history of trauma.51
In the cases reviewed of hand and upper extremity necrotizing fasciitis, only 8 of 54 (15%) had none of the aforementioned associations.33,52–58 One had Porphyria Cutanea Tarda,56 while the others had no significant past medical history.33,52–55,57,58 Of the remaining 46 cases, 31 had a single association, 8 (15%) had diabetes and an injury,59–66 and 6 (11%) were immunosuppressed with an injury.67–70 The remaining patient had three conditions associated with necrotizing fasciitis, including injury, diabetes, and IVDU.71
Presentation/Diagnosis
The presentation and diagnosis of necrotizing fasciitis pose a challenge, as symptoms may be unspecific. Generally, early symptoms of necrotizing fasciitis present as fever, erythema, edema, development of bullae, and pain out of proportion in the affected area.2,5–7 The most common symptoms were edema and pain, reported in 51 (94%)5,10,12–14,16–31,33–39,51–66,68,69,71,72 and 44 (82%)10–17,19–31,33–35,37–39,51,53,56–61,63–65,67–69,71 cases reviewed, respectively. Erythema was present in 24 (44%) patients,11,14,15,21–24,27,35,39,51,56,60–62,64–71 and 15 (28%) reported fever.11,14,19,24,27,31,33,34,37–39,51,55,70,72 Less commonly seen presenting symptoms included blisters/bullae, hypothermia, crepitus, malaise, ecchymosis or discoloration, hyperemia, drainage, numbness, confusion, and/or nausea and vomiting. Each were reported in five or fewer cases.5,14,15,17–19,29,31,37–39,52,58,59,62,72
Clinical suspicion of necrotizing fasciitis may be strengthened with the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) or diagnostic imaging [Table 3]. An LRINEC score of six or above has high specificity (84%), but a low sensitivity (59%), and a higher score indicates a greater mortality risk.5,73 An abbreviated LRINEC, using just a leukocyte count >15,400 cells/mm3 and serum sodium <135 mmol/L, has demonstrated a sensitivity of 90% and specificity of 76%.5 Only 4 (7.4%) reviewed cases reported a LRINEC score, with an average score of 7.75 (SD = 1.71).61,63,71,72 Three others provided the necessary data to calculate a score with a mean score of 7.67 (SD = 5.13).23,34,59 Adequate data was unavailable to determine LRINEC scores for the remaining 47 case studies examined.
Computed tomography (CT) may be valuable in diagnosing necrotizing fasciitis. On CT, absent enhancement of the thickened fascia indicating necrosis, asymmetric subcutaneous gas, fascial stranding, and fluid suggest necrotizing fasciitis.2,5 To quantify CT results, McGillicuddy et al.74 developed a scoring system demonstrating 86% sensitivity and 92% specificity for necrotizing fasciitis for scores >6. MRI has also been utilized, though enhancement and deep fascial thickening and fluid collection on T2 and contrast T1 images are found with other SSTI, not just necrotizing fasciitis.2,5
Wound cultures can be crucial for appropriate treatment; however, in 2 (3.7%) cases, cultures yielded no causative microbe,18,53 and in 2 (3.7%) others, no culture results were reported [Table 4].16,62 Of the remaining 48, 10 (19%) cases reported a polymicrobial infection.10,33,37,38,51,55,57,65,71,72 Overall, the most common infectious agents were gram-positive cocci, identified in 32 (59%) cases,5,10,11,14,15,21–24,27–29,31,33,34,38,39,51,52,55,58,59,65,67,69,72 followed by gram-negative bacilli in 21 (39%) cases.10,12,13,19,30,33,35,37,38,51,54,56,57,61,65,66,70,71 The most common pathogen was Group A streptococcus (GAS), reported in 15 (28%) cases11,14,21,23,24,27,29,31,39,52,55,67,69,72 followed by Vibrio in 6 (11%) cases.17,20,25,26,60,64 While bacteria were identified in a majority of cases, 4 (7.4%) cases identified fungi (Cryptococcus spp., Candida albicans, or Scedosporium apiospermum)38,68 and 1 (1.9%) identified Coxsackie virus.55
Treatment
Treatment of necrotizing fasciitis utilizes aggressive fluid resuscitation, empiric antibiotic coverage (for both gram-positive and gram-negative until speciation via culture), and emergent debridement.5,6,32 Despite an average of three debridements, amputation rates are 18-28%.5,7 Given the aggressive nature of the disease, treatment is time sensitive. Treatment within 24 hours of admission yields a 93% survival rate; by 48 hours, that falls to 75%.7
Among cases reviewed, 34 (63%) patients were administered three or fewer empiric antibiotics,5,11–13,15,19–29,33,34,39,52,55–59,63–67,70–72 while only 6 (11%) were administered four or more for empiric coverage.10,18,31,37,60,62 Additionally, 7 (13%) cases did not specify the empiric coverage30,38,51,52,68,69 was, and 7 (13%) did not report any empiric coverage.14,16,17,33,35,53,61 The most commonly administered medications for empiric coverage were glycopeptides and penicillin/beta-lactamase inhibitor combinations, each administered in 15 (28%) cases.10–13,15,18–21,24,25,28,29,31,37,39,52,55,58–60,62,63,65–67,70–72 Lincosamides were used in 12 (22%) patients.11,18,27,31,33,37,52,56,57,65,67,72 Penicillins were used in 11 (20%) cases,10,19,25,28,52,55–57,60,62,72 as were third-generation cephalosporins.5,11,15,22,24,26,28,31,37,52,64 Other medications reported include aminoglycosides, second and fourth-generation cephalosporins, monobactams, penems, oxazolidinones, nitroimidazoles, quinolones, and tetracyclines.
After obtaining cultures, 34 (63%) patients remained on three or fewer narrow-spectrum antibiotics.5,11–13,15,17–20,22–29,34,37,39,55–57,59,61,63–66,68,70–72 Penicillins and lincosamides were most often used for narrow antibiotic coverage, each used 13 times.11,15,17,22–24,27–29,31,39,55–57,65,72 Overall, the antibiotics used for narrow coverage were the same classes as those used for empiric coverage. In two cases, IVIG was used either in addition to or in place of antibiotic therapy.31,33 In another three cases, antibiotics were changed to appropriate antifungals after cultures demonstrated fungal growth.36,63,68
Along with aggressive medical management, 50 (93%) cases reported surgical intervention. Surgical intervention was not explicitly mentioned in two cases,38,70 and two specifically reported no intervention.37,60 Most patients had at least one debridement, 45 (83%), with an average of 2.09 (SD = 2.87) [Figure 2].5,10,11,13–15,17–31,33–35,39,51–59,62,63,65,67,69,71,72 Some patients underwent a fasciotomy, 8 (15%), with an average of 1.50 (SD = 0.76).12,13,16,20,31,36,61,66 Additionally, 7 (13%) patients underwent reconstruction with a free flap,11,21,31,51,56,69,71 16 (30%) underwent a split-thickness graft,11,12,15,17,26,31,51,53,56,61–63,66,67,69 1 (1.9%) had a decompression,17 1 (1.9%) had an osteotomy at the third digit,71 1 (1.9%) had a VAC placed,54 and 2 (3.7%) underwent incision and drainage.20,64
Outcomes & Complications
Complications after necrotizing fasciitis include amputation of the affected area, sepsis, septic arthritis, nosocomial infections, acute respiratory distress syndrome (ARDS), respiratory failure, renal failure, seizure, stroke, cardiac arrest, heart failure, and death.2,5
Patient follow-up ranged from six to 36 months, with an average follow-up period of 18 months. Most patients in the cases reviewed had either no or minimal long-term sequelae following their infection [Table 5]. No loss of function was reported for 24 (44%) patients after treatment,10,11,14,16,18,20,21,24,26,28,30,31,51,53,55,56,61–65,67–69 2 (3.7%) had mildly reduced motor function,15,66 and 1 (1.9%) had reduced motor and sensory function.34 Only 1 (1.9%) patient had a total loss of motor function after treatment.39 A total of 12 (22%) patients required amputation proximal to the infection site.5,12,13,17,22,23,29,33,57–59,71 Ultimately, 11 (20%) patients died from the infection.19,25,27,33,36–38,52,54,60,72
DISCUSSION
Necrotizing fasciitis, or necrotizing soft tissue infection, represents a rare but life-threatening SSTI requiring rapid intervention. This review compiled and synthesized case reports and series on hand, wrist, and forearm necrotizing fasciitis to identify trends and lessons in presentation, diagnosis, and treatment. While a meta-analysis would allow for more quantitative analysis of necrotizing fasciitis data, this would require data collection and reporting standardization to minimize the heterogeneity among studies. As such, a systematic review approach was utilized to allow for a comprehensive analysis accounting for the inherent variation in available data.
Current literature suggests a significant link with comorbidities, namely diabetes mellitus, immunosuppression, IVDU, and the development of necrotizing fasciitis.5,7,75–78 In fact, in one case series, 93% of patients had one of these three major comorbid conditions.75 In another case series, 59% had diabetes, and another 28% were immunosuppressed.76 Moreover, studies have found diabetes, in particular, to predict worse outcomes. Patients with poor glycemic control are at higher risk for necrotizing fasciitis, specifically type I polymicrobial infections.77 These patients are also at higher risk for requiring amputation secondary to their infection.77,78
This review found that injury, independent of comorbidities, is most associated with necrotizing fasciitis. In 43% of reviewed cases, patients presented with a history of recent trauma and no other comorbidities.5,10–30 Conversely, the most prevalent of the established big three comorbid conditions was diabetes, yet only 7.2% of cases presented with it as their only predisposition for necrotizing fasciitis.33–36 Immunosuppression was solely associated with 5.5%37–39 cases and IVDU in 1.8%.51 The same number of patients presented without any identifiable comorbidities as presented with diabetes, immunosuppression, or IVDU as sole risk factors (8, (14.81%)).33,52–58
The current understanding of the presentation of necrotizing fasciitis is that it can often mimic cellulitis or a mild inflammatory response to injury.79 As such, some studies have shown that a correct diagnosis on the first presentation may occur as little as 35% of the time.76 In fact, one study found many of these cases are often missed until the patient presents with septic shock.80 This review reaffirmed that the most common presenting symptoms include edema and pain, followed by erythema and fever.
Given the lethal consequences of a missed diagnosis of necrotizing fasciitis and the fact that some of the most common pathogens, namely GAS, Vibrio spp., and Pseudomonas spp. exist on opposite ends of the antibiogram, early recognition and intervention with broad-spectrum antibiotics is imperative. Leiblein et al. found that 93% of causative organisms identified at their hospital were susceptible to a combination of ampicillin, clindamycin, and metronidazole. They recommended empiric treatment using a penicillin/beta-lactamase inhibitor combination instead of just ampicillin.78 This review found the most commonly utilized empiric antibiotics include penicillins, penicillin/beta-lactamase inhibitors, vancomycin, and clindamycin; however, the combination of penicillin with clindamycin was only used in 7 cases.10,18,52,56,57,65,67
More important than empiric antibiotic administration is an early surgical intervention with fasciotomy and wide debridement. Literature suggests that delays in intervention can have deadly outcomes. Sunderland and Friedrich found that, on average, the time from presentation to surgical intervention in patients who survived was 25 hours, compared to 90 in those who did not.79 Similarly, Hsiao et al. found a mean time to OR of 1.5 days in patients who survived versus 3.9 in patients who did not.80 This review found an average of 0.50 days from initial presentation to OR in patients who died19,25,27,33,36–38,52,54,60,72 versus 0.71 days from initial presentation to OR in patients who survived.10,14,16,18,20,21,24,26,28,30,31,53,55,56,61–65,67–69,81 This difference could be due to the likely increased symptom severity in this group leading to a shorter time to the OR. However, the difference was significantly larger when comparing the time from symptom onset to clinical presentation. Patients who died from necrotizing fasciitis presented an average of 4.22 days after symptom onset19,25,27,33,36–38,52,54,60,72 compared to 1.87 in patients who survived.10,14,16,18,20,21,24,26,28,30,31,53,55,56,61–65,67–69,81
There is mixed data regarding the use of adjunct therapy in the treatment of necrotizing fasciitis. Riseman et al. found that in a study of 29 patients with necrotizing fasciitis, patients treated with hyperbaric oxygen (HBO) in addition to empiric antibiotics and surgical debridements had fewer debridements (1.2 vs. 3.3 in the non-HBO group, P < 0.03) and a lower mortality rate (23% vs. 66% in the non-HBO, P < 0.02).82 Similarly, Flanagan et al. found that patients who received HBO, empiric antibiotic therapy, and surgical intervention for cervical necrotizing fasciitis had shorter hospital stays than the overall study average, 9.1 ± 2.8 days compared to 11 ± 6.5 days.83 However, a review by Jallali et al. showed that the data regarding HBO as adjunctive therapy is inconsistent at best, with a need for more study of the potential risks of HBO.84 Similarly, a review by Levett et al. highlighted the lack of peer-reviewed randomized trial data to either support or refute the efficacy of HBO.85 Among cases reviewed here, only five utilized HBO, among which three resulted in no loss of function,51,56,62 one in reduced motor function,15 and one in a disarticulation.23
As an adjunctive therapy for severe infections, intravenous immunoglobulins (IVIGs) are sometimes used due to their immunomodulatory properties and ability to bind and neutralize bacteria and their exotoxins.3,86 However, further studies are needed as evidence supporting its clinical efficacy in treating necrotizing fasciitis is inconsistent.87,88 A meta-analysis by Parks et al. examining IVIG use in GAS toxic shock syndrome found that treatment was associated with a significant decrease in mortality from 34% to 16%.87 Contrary to this, a 2017 randomized trial of adjuvant IVIG treatment in necrotizing fasciitis caused by multiple pathogens found no difference in mortality among patients receiving the treatment.88 Among the cases reviewed in this study, only two used IVIG as an adjunct treatment to IV antibiotics. The first case resulted in successful graft healing and no loss of function,31 while the second resulted in a double limb amputation.33
There was one principal limitation of this study. Data and conclusions presented were subject to the variability in data provided in published case studies and series. While some provided thorough laboratory data and timelines, others offered brief overviews of case histories.
CONCLUSION
This review is one of the first systematic reviews of necrotizing fasciitis of the upper extremity. The two primary findings are 1) early recognition of the signs and symptoms of necrotizing fasciitis is imperative, and 2) aggressive management with empiric antibiotic coverage and rapid surgical intervention improves outcomes. Just as the differential for any patient reporting chest pain starts with a myocardial infarction, so should the differential for any patient with reported localized pain and swelling start with necrotizing fasciitis. Failure to assess for the disease on first presentation delays life and limb-preserving therapy. Additionally, given the wide variety of pathogens that can be responsible for the infection, full-spectrum antibiotic coverage (i.e., piperacillin-tazobactam and clindamycin, plus either a tetracycline or macrolide antibiotic for atypical coverage) would be advisable. Future studies should work to identify more definitive trends in outcomes based on specific antibiotic regimens and discern what role, if any, adjunct therapy such as hyperbaric oxygen has in treating necrotizing fasciitis.
Declaration of conflict of interest
The authors do NOT have any potential conflicts of interest in the information and production of this manuscript.
Declaration of funding
No funds were received in the production of this manuscript.
Declaration of ethical approval for study
This study was determined to be exempt from IRB approval by the Thomas Jefferson University Institutional Review Board.
Declaration of informed consent
The authors declare that there is no information in the manuscript that can be used to identify patients