Introduction
Approximately 500,000 total hip arthroplasties are performed annually in the US, where 4.1% end up with a femoral periprosthetic fracture (PPF) complication.1,2 Femoral PPFs present challenges to orthopedic surgeons regarding fixation and management.3 Despite advancements in current techniques and technology, the incidence of PPFs is increasing.4,5 This increase has been attributed to the aging of the population (increasing life expectancy and prevalence of senile osteoporosis), the increasing number of primary and revision hip arthroplasties, and the increasing use of uncemented femoral stems.6,7 Currently, PPF is the most common indication for femoral implant revision for uncemented femoral stems, the second most common indication for any revision total hip arthroplasty (THA), and one of the most common indications for reoperation after a revision THA.6,8–10
Surgical management of PPFs is technically demanding, given the often-poor bone quality, altered anatomy, and the need to manage both the prosthesis and the fracture.11,12 PPF treatment primarily focuses on whether the femoral stem is stable or unstable.13 With stable stems, treatment focuses solely on fracture fixation.13,14 However, with unstable stems, treatment relies on both the revision of the femoral stem and the fixation of the fracture.13,15 Using the Vancouver classification of PPF types B1 and C encompass the fractures with a stable femoral stem that require internal fixation.13
Vancouver type C fractures (distal to a fixed proximal stem) account for around 10% of all periprosthetic fractures.16,17 They are known to be the most complex to manage and are associated with the most complications.18,19 Complication rates of up to 55% have been reported following surgical fixation of Vancouver type C femoral fractures, particularly in cases involving non-union, malunion, and hardware failure.17,20–22 Some authors have suggested the utilization of a proximal, transitional unicortical locking screw, whereas others advocate for the mere overlapping of the plate with the intramedullary implant.23,24 Thus, alternative fixation hardware, such as cerclage cables and unicortical locking screws, must be used to secure the plate to the proximal segment of the bone.25
Therefore, this study aims to compare the biomechanical performance of four plate fixation configurations used to repair Vancouver type C periprosthetic femur fractures. We hypothesize that using a bicortical screw in the construct will have the highest stiffness, and cerclage cables will not have an effect when bicortical screws are utilized. The clinical and biomechanical relevance of this study lies in the fact that the optimal solution remains elusive for this injury pattern.
Methods
Construct Configuration
Six large adult 4th generation biomechanical low-density femur Sawbones (Model #3406-5; Vashon Island, WA, USA) were used to conduct this study. Synthetic femurs were used as they offer many advantages over human cadaveric specimens and significantly reduce inter-specimen variability.26 The femoral head was replaced by a size 9 collared proximal femur stem hemiarthroplasty prosthesis (Stryker, Portage, MI, USA) with a unipolar 50 mm head secured in the model with polymethyl methacrylate (PMMA). To recreate a comminuted Vancouver type C periprosthetic femur fracture, a 1 cm gap was created by segmenting the femurs into two below the tip of the femoral stem. A stainless steel 18-hole 336 mm plate (316L, Synthes, Monument, CO, USA) was attached to the distal fragment with three bicortical screws (hole locations 1, 3, 5). The proximal fracture fragment was evaluated with the following four configurations (Table 1): A) Three unicortical screws and 11 bicortical screws; B) 3 unicortical screws, two cerclage cables, and one bicortical screw; C) 3 unicortical screws with two cerclage cables; and D) 3 unicortical screws. All unicortical screws were placed in holes 14, 16, and 18. It should be noted that all specimens were tested under each condition consecutively, starting with condition A and finishing with condition D.
Mechanical Testing
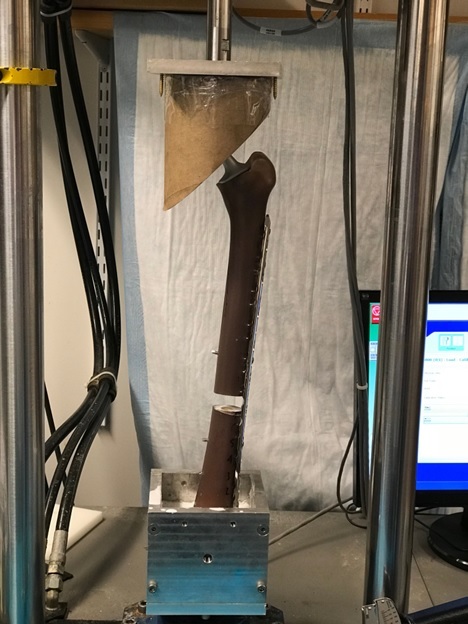
To evaluate the mechanical strength of each Vancouver type C plate fixation configuration [Figure 1], the PPF specimens underwent axial compression and four-point bending tests to determine axial and flexural construct stiffness. Each specimen was first loaded in axial compression and then in 4-point bending, with all experiments conducted on the same mechanical testing system (Instron 8511, Norwood, MA, USA).
Axial Compression
To simulate a single-leg stance, each specimen was oriented in 15° of adduction in the frontal plane and aligned vertically in the sagittal plane. Specimens were mounted distally in a custom-built testing apparatus, where the femur was fixed using PMMA [Figure 2]. Proximally, the femoral head was inserted into a custom conforming cup free to rotate inside the cup [Figure 2]. To evaluate construct stiffness, each specimen was subjected to 250, 500, and 1000 N loads at a load rate of 1.0 mm/s until the maximum force was obtained.27 Testing for each specimen started with construct A and finished with construct D. Each Test was carried out three times so that the stiffness for each case was the average of the three trials to verify repeatability and ascertain accuracy. Stiffness was calculated as the slope of the force-displacement curve within the linear elastic region. Although the load levels were low compared to physiological activity, they were chosen to prevent permanent damage to the specimens, as they were to be tested multiple times.27
Four-point Bending
Following axial compression testing, each femur was mounted horizontally with the plate facing down in a custom testing apparatus for four-point bending [Figure 3]. The plate supports were spaced 350mm apart, the loading pins were 150 mm apart, and they were placed equidistant from the osteotomy site. A vertical load of 500 N was applied to the mid-shaft of the femur on each side of the osteotomy site at a rate of 1mm/s until the maximum load was reached. Stiffness was calculated as the slope of the force-displacement curve within the linear elastic region. This procedure was repeated for constructs A to D on each specimen, with three trials taken per construct, and the average value of the three trials was taken as the stiffness. Similarly, the load was chosen to avoid permanent damage to the specimens as they were to be tested multiple times.
Statistical Analysis
A descriptive analysis was presented as the mean and standard deviation for each condition. Shapiro-Wilk test was used to assess the normality of the data for each condition. Construct stiffness was compared to understand whether there was a significant difference between various combinations of screw fixation with or without using cerclage wire on the overall mechanical stiffness during 4-point bending or axial loading tests. One-way repeated measure analysis of variance (ANOVA) with a Greenhouse-Geisser correction was used to compare the effect of each configuration on the stiffness as the outcome of interest. Post-hoc pairwise comparisons were made and adjusted by the Tukey multiple comparisons test to find which conditions were significantly different [Table 2]. Statistical analysis was performed using GraphPad Prism (version 9.3.1 for Windows, GraphPad Software, San Diego, CA, USA). Two-tailed p-values less than 0.05 were considered significant.
Results
Conditions A and B had comparable stiffness values, while their stiffness was greater when compared to conditions C and D under axial and bending loads [Figure 4]. One-way repeated measures ANOVA tests revealed significant differences in mean stiffness between the two groups during axial or 4-point bending tests [Table 2]. Conditions A, B, and C demonstrated considerably higher stiffness during the 4-point bending test than condition D. Furthermore, conditions A and B showed significantly higher stiffness than condition C [Figure 4a]. During axial testing, condition A demonstrated significantly higher stiffness than condition D at 500N and 1,000N loads but not at 250N. Condition B significantly outperformed condition C in all testing loads and showed significantly higher stiffness than condition D at 500N and 1000N forces [Figure 4b-d].
Discussion
This study aimed to identify the most effective fixation construct for complex periprosthetic type C type C fractures in THA. Specifically, we aimed to determine the fixation technique demonstrating the greatest mechanical strength when utilizing mono-cortical screws in the proximal segment, augmented by either bicortical screws, cerclage wire, or a combination of both. These constructs were selected based on their relevance in current clinical practice and their potential to offer enhanced mechanical stability. Our study demonstrated that adding bi-cortical screws to the proximal fragment significantly improved the mechanical strength compared to mono-cortical screws alone or incorporating cerclage wire. This finding confirmed our hypothesis that bi-cortical screws provide greater mechanical strength in such fractures. However, the difference in mechanical strength was not statistically significant when a combination of bi-cortical and mono-cortical screws was compared with a combination of bi-cortical and mono-cortical screws plus cerclage wire. This study provides insight into the biomechanical characteristics of different fixation constructs, which can aid surgeons in making informed decisions for managing complex type C periprosthetic fractures of the femur following total hip arthroplasty.
PPFs present unique challenges for orthopedic surgeons in terms of management. Limited cortical fixation options, poor bone quality, cement mantles, stem, and stress risers are some of the challenging issues that surgeons would consider when encountering PPFs.14 More specifically, these challenges become more apparent when experiencing Vancouver type C PPFs, of which the femoral stem is stable and retained. Plate fixation is the main mode of fixation used in type C PPFs. Various fixation constructs are available, including locking plates, bicortical screws, unicortical locking screws, and cerclage wires and cables. However, consensus on the optimal proximal construct fixation in type C PPFs is lacking.
Our study demonstrated that bicortical screws in the proximal construct of comminuted type C PPFs provide greater biomechanical stability during axial and bending loads. A study by Dennis et al.28 focused on elucidating the biomechanical properties of different plate fixations in periprosthetic femoral shaft fractures after total hip arthroplasty using the type III Cooke fracture pattern (equivalent to the type C Vancouver fracture used in our study classification). In contrast to our study, their fixation constructs did not include bicortical screws in the proximal fragment. Their results demonstrated that plate constructs with proximal unicortical screws and distal bicortical screws, as well as those with proximal unicortical screws, proximal cables, and distal bicortical screws, exhibited significantly higher stability in axial compression, lateral bending, and torsional loading. Although both studies contribute valuable insights into the biomechanical behavior of plate fixations, our study highlights the importance of bicortical screw engagement in the proximal fragment, which may have contributed to the superior biomechanical performance of specific fixation techniques in our experimental setup.
Stevens et al. compared three wiring techniques for cerclage plating in type C periprosthetic fractures using synthetic femurs. The three techniques included simple cerclage (single wrap around the bone and plate), double cerclage, and double cerclage with a plate insert. Through biomechanical tests, the researchers found that the double cerclage with plate insert technique outperformed the other two methods regarding fixation strength and stability.29 Schmotzer et al. explored the efficacy of various fixation techniques using cementless implants in transverse osteotomy of cadaveric femurs. The study encompassed six fixation methods applied to seven cadaveric femurs to simulate clinical scenarios. Among the fixation techniques assessed, a plate with proximal unicortical screws demonstrated the most favorable fixation strength until the pull-out of the proximal screws.30
The study conducted by Lever et al. examined the mechanical stability of various fixation techniques utilized for periprosthetic femoral fractures near the tip of total hip arthroplasty. A total of twelve pairs of human cadaveric femurs were utilized in the study, wherein the left femur of each pair was subjected to the cemented insertion of the femoral component of a complete hip implant. Type C femoral fractures were induced in the femurs, followed by implementing three different fixation methods for later repairs: the Zimmer Cable Ready System, the AO Cable-Plate System, and the Dall-Miles Cable Grip System. Lever et al. concluded that screw-plate systems demonstrated superior mechanical stability compared to cable-plate systems in cases of periprosthetic femur fractures distal to the tip of the stem.31
In the study by Zdero et al., the biomechanical performance of four different fracture fixation constructs was evaluated using twenty synthetic femora subjected to axial compression, lateral bending, and torsion tests. They concluded that a combination of nonlocking cable-plate with an allograft strut, cables, and nonlocking screws exhibited the highest stiffness for treating a periprosthetic fracture around a stable femoral component of a total hip replacement compared with locked plate with locked screws, locked plate with cables and locked screws and nonlocking cable plate with cables and nonlocked screws.32 The clinical relevance of these findings suggests that a locked plate should be used with caution as a stand-alone treatment for fixing periprosthetic femoral shaft fractures following total hip arthroplasty. According to Kubiak et al., overlapping the stem of a total hip implant with a locking compression plate in Vancouver type C fracture leads to reduced strain on the construct and increased load to failure compared to other fixation methods.33
While acknowledging that the biomechanics of the upper extremity differ from the lower extremity, Gupta et al. investigated the impact of adding cerclage wiring to the bicortical fixation of locking plates. The results demonstrated that isolated screw constructs, without adding cerclage wires, exhibited increased resistance against torsional movement, bending, and shear compared to constructs with cerclage wires. Interestingly, the hybrid construct, which combined both screw and cerclage elements, did not provide significant changes in stability compared to the isolated screw construct.34 Given the potential risks related to tissue stripping and nerve damage frequently associated with using cerclage wiring, it is imperative to exercise caution when contemplating the application of cerclage wires in a comparable clinical context.
In a recent study conducted in 2022, Pierret et al. aimed to compare different fixation methods in synthetic osteoporotic femoral shaft fractures. Their investigation centered around evaluating the mechanical strength of bicortical screw fixation, which is currently considered the reference standard. Similar to our study, bicortical screw fixation demonstrated significantly greater mechanical strength than three of the four mono-cortical screw constructs tested.35 However, what sets their study apart is the use of mono-cortical screw fixation combined with double cerclage. Intriguingly, their evaluation found no significant difference in mechanical strength compared to bicortical screw fixation. This finding suggests that mono-cortical screw fixation with double cerclage may present a viable alternative to bicortical screw fixation, particularly in cases where an implant in the intramedullary canal precludes bicortical screws.
Lewis et al. showed that bicortical constructs could resist greater torsional forces than unicortical screws and cerclage cables and greater axial loading than cerclage cables.36 In line with the study by Lewis et al., Hoffmann et al. showed the construct with bicortical screws only had the greatest load to failure and stiffness during torsional/sagittal bending than constructs that had unicortical screws with cerclage and cerclage alone.37 However, during axial loads of 500N, the cerclage-only constructs had the highest stiffness compared to the other groups, and no significant difference in construct stiffness was reported between the groups during lateral bending forces.37 In our study, at axial loads of 500N, the presence of bicortical screws in the proximal construct with unicortical screws and cerclage wires had a significantly greater stiffness than unicortical screws with cerclage and unicortical screws only constructs, which is in line with the study by Lewis et al. However, it is important to note that in their study, the significant difference observed during axial loading was in the proximal construct that contained only bicortical screw fixation, which is different from our study, where there was a combination of unicortical screws, bicortical screw, and cerclage cables. In addition, the bicortical screw groups had significantly greater stiffness during 4-point bending than the unicortical and cerclage cable groups, in contrast to Hoffmann et al.'s study, which showed no significant difference among the fixation groups. The difference in results can be attributed to the difference in proximal construct configuration, as Hoffmann et al. only used bicortical fixation screws without combining cerclage cables and unicortical screws. In addition, the fracture geometry in Hoffmann et al.'s study was oblique, and the force applied during lateral bending was applied through the femoral head rather than around the fracture site, as was done in this study with 4-point bending.
Cerclage wires or cables have long been used for fracture fixation in PPFs. Their common use in PPFs originates from bypassing the need to pass screws through the bone in the vicinity of the cement or the femoral stem, which can be challenging.38,39 However, they risk disrupting the blood supply to the bone when stripping the periosteum to pass the wire and possibly injuring neurovascular structures.40–42 Furthermore, their use has been questioned since their contribution to overall construct stiffness is inconclusive in the literature. Lewis et al. showed that cerclage cable-only constructs had significantly lower stiffness than all other construct groups.36 However, Gordon et al. showed that cerclage cables had significantly higher stiffness than screw fixation during axial loads.25 Due to the variability of study outcomes, surgeons have shied away from their sole use and have augmented their proximal constructs with screw fixation. Thus, our study analyzed the effect of cerclage wires in combination with unicortical fixation and bicortical fixation to evaluate its contribution to the overall construct stiffness. The unicortical-screw-only construct was shown to have the least amount of construct stiffness compared to the other groups. This was also confirmed by Graham et al., which showed that proximal unicortical locking screws alone did not provide enough stiffness to proximal constructs.43 However, we saw that augmentation with cerclage cables increased the construct stiffness in axial and bending loads but was only significant during bending loads. Hoffmann et al. showed that combining unicortical screw and cerclage cables had significantly greater stiffness than cerclage-only and bicortical-only constructs after cyclic axial loading.37 Furthermore, a study conducted by Shah et al. showed that combining unicortical screws and cables had greater stiffness than cables alone or screws alone.44 Thus, from our study and other studies in the literature, cerclage cables or wires might have more impact in combination with unicortical screws rather than bicortical screws. In addition, they may have a protective effect on proximal constructs during cyclic loading, as shown by Hoffmann et al .37
While our study and others have provided valuable insights into the mechanical stiffness and stability of different fixation systems for periprosthetic femoral fractures, it is crucial to emphasize that mechanical stiffness alone should not be regarded as the exclusive or primary determinant of the clinical success of fracture fixation procedures. Clinical success in managing periprosthetic femoral fractures involves a multifaceted evaluation beyond mechanical properties. While mechanical stiffness is essential to fixation stability, it may not necessarily translate to better clinical outcomes if other factors, such as bone-implant interface biology and the potential for secondary displacement or nonunion, are not adequately addressed.
There are several limitations associated with this study. One primary limitation is the small number of samples. Further research with a larger sample size is necessary to assess the findings more precisely. Another drawback of the study is the use of a regular LC-DCP plate instead of an anatomical cable plate, which has the potential to induce alterations to the obtained results. Most cable plates are designed as anatomical femoral plates, rendering them incompatible with type C fractures due to their relatively short length. Synthetic femur models were used as a substitute for cadaveric bones to avoid natural variability in bone geometry and quality and to improve equivalence.
Nevertheless, it may not reflect actual bone biomechanics. The effect of fatigue loading was not investigated. Fatigue failure in fixed PPFs occurs approximately after 22 months of fixation.45 Previous studies to replicate fatigue loading have used fast-tracked timelines. Still, they do not reflect the influences of healing and callus formation on the biomechanical properties of the healing PFFs. We could not accurately simulate all physiologic forces on the femur. This study’s setting does not represent the effect of soft tissues such as muscles and ligaments, which may provide additional stability to the fracture site and alter the biomechanical characteristics. This study aimed to compare the relative stiffness between constructs instead of an ideal value for enhancing fracture healing, a trade-off between construct stiffness and biological factors. Increased stiffness does not equate to an optimum healing situation.
Conclusion
In conclusion, using bicortical screws in the proximal construct of Vancouver type C PPFs increases construct stiffness in axial and bending loads. Though controversial, the use of cerclage cables might have a place for construct augmentation when using only unicortical screws or a combination of unicortical and bicortical screws, and its effects might be related to maintaining the longevity of the construct rather than increasing its stiffness during acutely applied loads.
DECLARATION OF CONFLICT OF INTEREST
The authors declare no conflict of interest.
DECLARATION OF FUNDING
AO Foundation Fellows Research Grant
DECLARATION OF ETHICAL APPROVAL FOR STUDY
The Institution requires no ethical approval for cadaveric studies.
DECLARATION OF INFORMED CONSENT
Not applicable




_with_a_greenhouse-geisser_correction.png)


_with_a_greenhouse-geisser_correction.png)