INTRODUCTION
Since Charnley’s uniplanar external fixator compression device in 1951, different techniques have been developed for joint ankle arthrodesis.1 Current techniques utilize an open or arthroscopic approach with successful clinical outcomes.1,2 The open techniques allow for easier placement of plates, bone grafts, and correcting malalignment2; however, the complication rate has been reported to be as high as 26.9%.3 Conversely, the arthroscopic approach is less invasive and has demonstrated similar union rates to the open approach.4–7 While the arthroscopic approach is successful, it is not recommended for patients with severe arthritis, ankle deformity, and malignment.4
We propose a novel technique, designed by one of the senior authors, using a tibiotalar arthrodesis nail system. This curved nail system employs a minimally invasive procedure, providing compression and rigid fixation of primary ankle fusions. The intramedullary nail is placed through the medial side of the talus and across the ankle joint into the tibia, achieving fusion at the tibiotalar joint without violating the subtalar joint and avoiding heel incisions. Similar to the tibiotalocalcaneal (TTC) intramedullary nail, this system’s nail can load share, allowing early postoperative weight-bearing.8 This paper aims to explain the technical pearls of the Shotel Ankle Arthrodesis Nail System and present the short-term outcomes of our patients who received the Shotel Nail.
METHODS
Indications for this technique include isolated advanced tibiotalar arthritis that has failed nonoperative management.8 Absolute and relative contraindications include insufficient talar height, a pilon fracture extending beyond the metaphysis, active infection, avascular necrosis of the talus with collapse, severe deformity that requires osteotomies, insufficient blood supply or quality of bone, and metal allergies.8
The Surgical Technique9
The patient is placed in a supine position on a radiolucent operating table.
-
The ankle joint is prepped open or arthroscopically with or without bone graft (per surgeons’ preference).
-
Provisional fixation: Achieved utilizing 2.4 mm pins posteromedially and anterolaterally with the joint in the optimal position (neutral flexion, 0º-5º valgus, and 5º-10º external rotation) [Figures 1A-B].
-
An incision is made from the tip of the medial malleolus to the navicular tubercle along the posterior tibialis tendon.
-
The tendon is retracted inferiorly to expose the insertion site. This is located proximal to the articular cartilage of the talar head and superior to the spring ligament.
-
Entry portal: Using fluoroscopy, a straight entry awl is advanced while aiming superolateral and slightly posteriorly. The awl should exit slightly lateral to the center of the talar dome on the radiographic anterior-posterior view and parallel with the longitudinal axis of the tibia on the lateral view. Of note, a drill can alternatively be used for this step after an awl creates the entry portal at the insertion site [Figures 2A, 2B, and 2C].
- A mallet is used to advance a curved trocar through the talus across the joint line into the tibia, creating a curved pathway [Figure 3].
-
Next, the rigid stainless steel guide wire is inserted into the prepared curved pathway.
-
The diameter of the curved pathway is enlarged with a flexible reamer [Figures 4A and 4B].
- An appropriately sized Shotel Nail attached to a drill guide is inserted while the nail depth is adjusted so that the transarticular screw trajectory is aimed toward the lateral process of the talus [Figures 5A and 5B].
-
The first proximal screw is placed using the drill sleeve and drill guide. Four proximal screw holes are provided on the nail.
-
To achieve compression, the compression sleeve is moved into position by manually turning the compression nut.
-
Temporary fixation pins are removed.
-
The joint is compressed with the compression sleeve by tightening the nut with the provided wrench.
-
The trans articular screw is placed using the drill guide.
-
The talar screw is placed using the drill guide.
-
One, two, or three additional proximal screw(s) are placed.
-
The drill guide and compression sleeve are removed, the nail cap is placed, and the wound is closed in layers [Figures 6A and 6B].
RESULTS
Ten patients in our series underwent Shotel Nail implantation [Table 1 and 2]. Patients had a mean follow-up of nine months. Initial FAAM (Foot and Ankle Ability Measure) scores improved from 40 to 50 at the most recent follow-up. Visual analog scores decreased from 6.7 at the initial visit to 4.2 at the most recent visit. PROMIS (Patient-Reported Outcomes Measurement Information System) mental health scores changed from 15 to 14, and PROMIS physical health scores varied from 11 to 13. There were no conversions to a total ankle arthroplasty. All patients had a successfully fused ankle arthrodesis at the last follow-up.
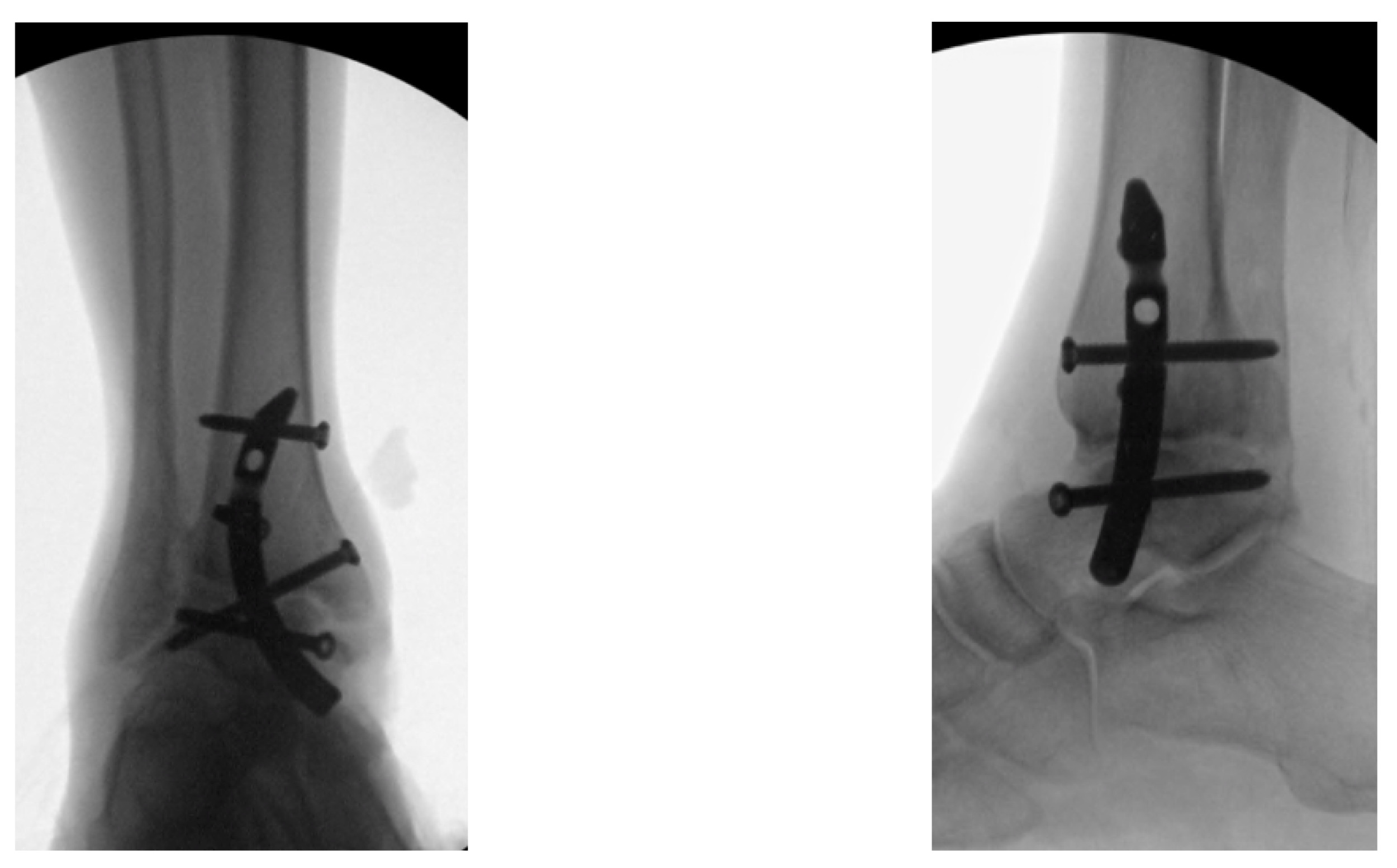
Examples of postoperative images of the Shotel Nail are included in [Figures 7A-C].
Postoperative Management
Surgeries were performed on an outpatient basis. Postoperatively, the patients were placed in a well-padded splint or a cast and were allowed toe-touch weight-bearing status. At the first follow-up after 10 to 14 days, sutures were removed, and the patients were transitioned to a controlled ankle movement walker boot.10 Patients were followed every four weeks until the union was achieved.
DISCUSSION
Many different surgical techniques have been described for ankle arthrodesis, which can be categorized into external fixation and internal fixation (plates, screws, or intramedullary nails) via open or arthroscopic approaches.11 We believe that the Shotel Nail System and technique offers a unique method by combining the advantages of existing methods while minimizing disadvantages and associated complications. Prior literature has shown that compression is essential when performing ankle arthrodesis.12 The Shotel Nail achieves compression through a proximal locking screw that acts as an anchor to compress the tibiotalar joint along the arc of the Shotel Nail.
The Shotel Nail System is minimally invasive and allows for early weight-bearing. It provides the stability and stiffness found in an intramedullary nail. Our technique improves upon TTC nail arthrodesis by mitigating the risk of neurovascular injury and sparing the subtalar joint, which has been hypothesized to allow for compensation for the misalignment associated with tibiotalar arthritis.5
The three-screw technique for ankle fusion is a common technique because it is simple and cheaper than plates. The technique involves tibiotalar arthrodesis. The three-screw technique has been reported to have high union and satisfaction rates.13 Plates are used when increased stiffness to protect arthrodesis is desired. The use of plates and compression screws together increases the stiffness of the construct compared to plates or screws alone.14 The Shotel Nail is a stiff intramedullary construct that allows earlier weight-bearing compared to plates and screws or the three-screw technique. There are various plate options at the surgeon’s disposal, but their use requires extensive dissection, which may increase the risk of infection and damage to surrounding tissues.15,16 The Shotel Nail can be placed with a small incision, avoiding the need for extensive dissection and the risk of damage to surrounding structures.
This proposed technique provides a viable alternative for end-stage isolated tibiotalar arthritis and a foundation for future investigation to uncover the reproducibility, effectiveness, and clinical outcomes in a larger patient population. Additionally, given the minimally invasive nature of the Shotel technique, it may be a better option for later conversion to total ankle replacement. Conversely, the Shotel Nail System can be a potential alternative to TTC nail for arthrodesis following failed ankle arthroplasty.
The medial approach to the foot and ankle has shown favorable results with other surgical techniques, such as hindfoot arthrodesis. The exposure allows for adequate alignment of the talus, especially for those deformities associated with flatfoot.17,18 Studies have been conducted that demonstrate low-rate skin complications.17,19 Important anatomic structures medial to the ankle are at risk with a medial approach. The insertion point of the Shotel Nail, being more anterior on the talus, minimizes the risk of damage to the more posterior neurovascular structures. There is a potential concern for disrupting the blood supply to the talus. However, there have been few reported cases of osteonecrosis of the talus using a medial approach. Of the cited cases in the literature, many involve screws placed in a posterolateral position in the talus for hindfoot arthrodesis.20 The placement of the Shotel Nail avoids the lateral portion of the talus and thus can be reasoned to have minimal risk of disrupting the blood supply. Miller et al. described a rich anastomotic network, which may suggest why the disruption of one or two of the vascular supplies to the talus does not necessarily result in necrosis of the talus.21 Rohm et al. discussed that the medial approach does not compromise the vascular supply to the talus due to the incidence of nonunion being similar to what is reported in the literature using other approaches, and avascular necrosis has rarely been reported.20 Given the small size of the incision made for the Shotel Nail technique, it is likely that the results would be similar. Further research must be conducted to assess functional outcome scores, long-term outcomes, and potential complications of the Shotel Nail.
CONCLUSION
Patients undergoing tibiotalar arthrodesis using the Shotel Nail have acceptable outcomes. Considering this technique as a minimally invasive intervention, we believe that soft tissue complications are less than conventional open techniques. The Shotel Nail System offers an innovative perspective on surgical treatment of symptomatic end-stage tibiotalar arthritis. The technique and implant combine the advantages of conventional methods while mitigating some of the commonly associated disadvantages with more extensive arthrodesis by sparing the subtalar joint. With further investigation, we believe our approach and implant provide the foundation to revolutionize tibiotalar arthrodesis.
Declaration of Conflict of Interest
Dr. Marrero owns stock in the company that owns the intellectual property that governs the technology described in this paper.
Declaration of funding
The authors received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of ethical approval for the study
The Institutional Review Board granted ethical approval for conducting this study.
Declaration of informed consent
No information in the submitted manuscript can be used to identify patients.
Acknowledgments
The authors have no acknowledgements to report.





._the_shotel_nail_on_locking_jig_with_cross-locking_trocar._b_(right)._intraoperat.png)






._the_shotel_nail_on_locking_jig_with_cross-locking_trocar._b_(right)._intraoperat.png)