INTRODUCTION
A variety of modalities are utilized in Total Hip Arthroplasty (THA) to achieve analgesia, including oral non-steroidal anti-inflammatory drugs (NSAIDs), local anesthetics, peripheral nerve blocks, and opioid pain relievers.1 Studies have shown that regarding postoperative analgesia, orthopedic surgeons in the United States rely more on opioids for pain relief compared to those in other high- and low-income countries.2,3 To combat the rising morbidity concurrent with the use of opiates for analgesia, opioid-sparing pain management strategies have become a new focus of research. One such therapeutic recently investigated as a local anesthetic is liposomal bupivacaine.
Local anesthetics such as bupivacaine and ropivacaine are effective forms of perioperative analgesia in THA.4 They are utilized as periarticular injections or peripheral nerve blocks to mitigate post-operative pain. Liposomal bupivacaine is a novel formulation that delivers bupivacaine through multivesicular liposomes, allowing for extended-release and longer analgesia.5 In 2011, liposomal bupivacaine was approved for pain control in hemorrhoidectomies and bunionectomies.6 The Food and Drug Administration (FDA) then expanded its indication to local surgical infiltration in 2015.7 Multiple studies have been conducted to evaluate its efficacy in THA.8–16 This systematic review aims to assess the current literature to determine whether incorporating liposomal bupivacaine as a local anesthetic in perioperative pain control strategies improves pain scores and reduces total opioid consumption in adults undergoing THA compared to other used local anesthetics.
METHODS
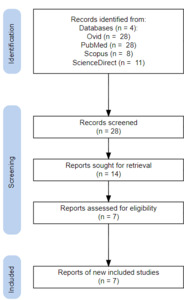
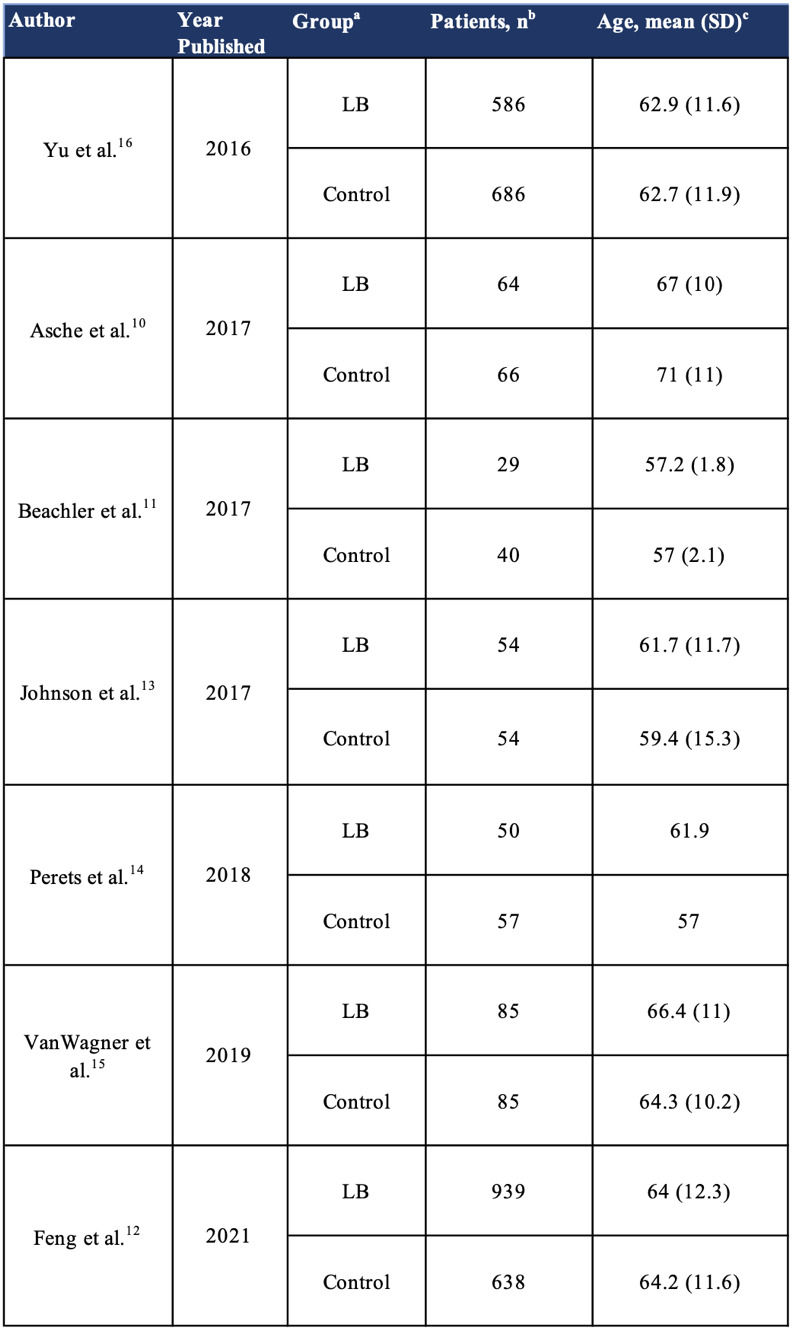
A systematic review was performed using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The systematic search was conducted in November 2022 using Ovid Medline, PubMed, Scopus, and ScienceDirect databases with search terms “Liposomal Bupivacaine OR Bupivacaine Liposomal” and “Hip Arthroplasty.” A total of 28 studies were identified based on title and abstract for full-text review [Figure 1]. Studies were screened based on inclusion criteria of 1) prospective randomized control trials or retrospective cohort studies, 2) conducted after 2015 FDA expansion of liposomal bupivacaine indication to local surgical infiltration, 3) compared liposomal bupivacaine as a periarticular injection to other local anesthetics used as a periarticular injection, and 4) available in English.7 Any meta-analyses, systematic reviews, case reports, and letters to the editor were excluded from this systematic review. Articles were screened independently by two investigators (RM, MK). Any inconsistencies were discussed between the investigators to reach a consensus. Discrepancies in article eligibility between the two investigators were resolved by a third investigator (SR). The systematic search resulted in 28 abstracts identified. After a full-text review, seven articles, comprised of two Level I and five Level III evidence, with a total of 3433 patients, were included in this study [Table 1].10–16 Primary outcomes included pain scores and total opioid consumption. Secondary outcomes of mobility scores, time to ambulation, length of stay, incidence of adverse events, and cost were also reviewed when available. Pain scores between LB and control groups were assessed in the immediate period (24 hours), short-term period (72 hours), and long-term period (>30 days). Opioid consumption was directly reported in morphine milligram equivalents (MME) or converted to MME for analysis.
RESULTS
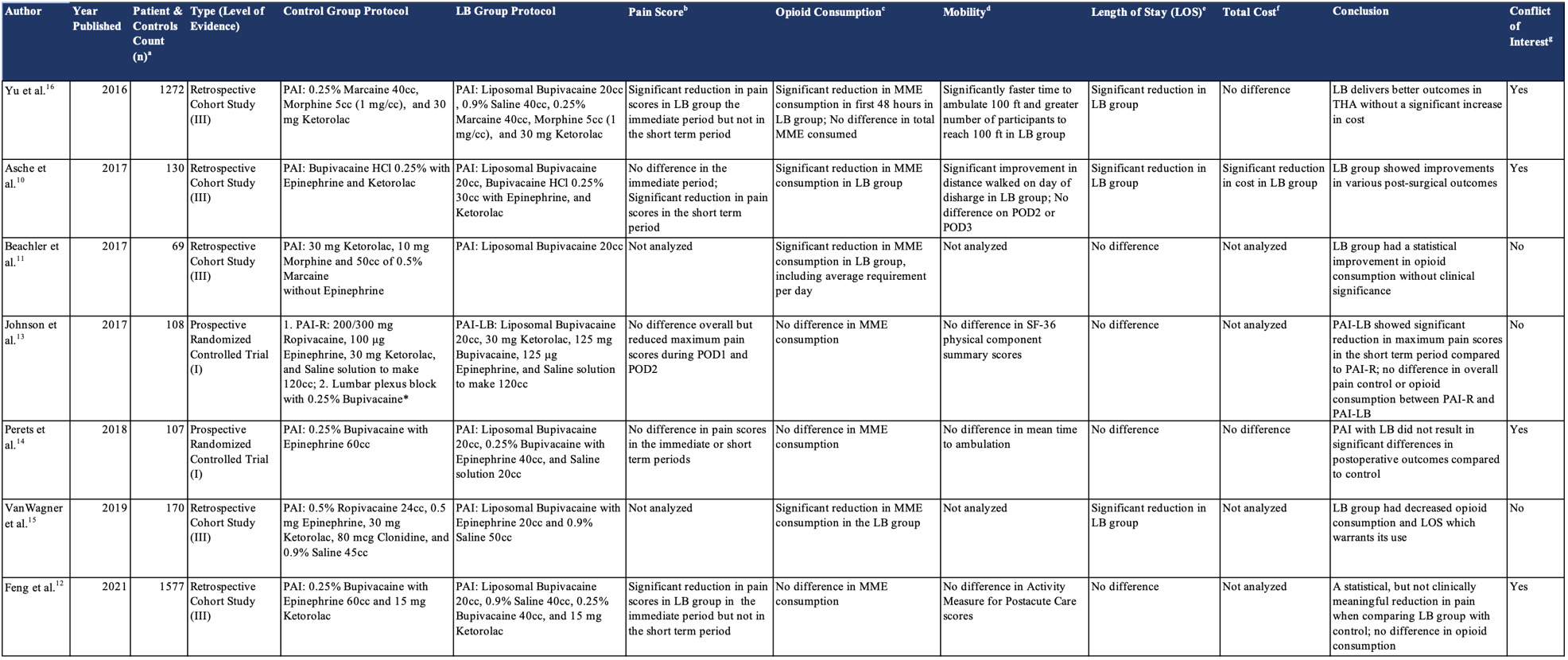
The studies compared periarticular injections with liposomal bupivacaine to another local anesthetic such as bupivacaine [Table 2]. All studies used a single dose of LB in the experimental groups.10–16 The following outcomes of interest were evaluated.
Pain Scores
Five articles compared pain scores in the LB group with a control group.10,12–14,16 In the immediate postoperative period, three studies showed no significant difference in pain scores, and two showed a significant decrease in pain scores when comparing the LB group to the control group.10,12–14,16 In the short-term period after THA, three studies showed no significant difference in pain scores between the LB and control groups, and two studies showed significantly reduced pain scores in the LB group.10,12–14,16
Opioid Consumption
All seven articles compared total opioid consumption in the liposomal bupivacaine group with a control group.10–16 Four studies showed no significant difference in total opioid consumption between LB and control groups.12–15 Three studies showed significant reductions in total opioid consumption among the LB group compared to the control group.10,11,15 Beachler et al. found significant decreases in both total opioid consumption as well as average opioid requirement per day.11
Mobility
Five articles compared functional outcomes between LB and control groups, such as mobility and time to reach ambulation milestones.10,12–14,16 Yu et al. showed a significantly faster time to ambulate 100 feet within the LB group compared to the control.16 The other four studies found no significant difference in their reported functional outcomes.10,12–14
Length of Stay
All seven articles compared the length of stay between the LB and control groups.10–16 Three studies reported significant decreases in length of stay within the LB group compared to the control group.10,15,16 Four studies found no significant difference in length of stay between LB and control groups.11–14
Adverse Events and Readmission Rates
Four articles compared the incidence of adverse events or readmission rates, and all four found no significant differences between the LB and control groups.10,13,14,16
Total Cost
Three studies compared the total care costs accrued during the length of stay between the LB and control groups. Perets et al. and Yu et al. reported no significant difference between both groups, and Asche et al. found a significant reduction in cost within the LB group.10,14,16
DISCUSSION
Total hip arthroplasty allows patients to regain hip mobility, perform daily functions, and lead a life with less pain.17 LB can reduce pain and opioid consumption after surgery; thus, its efficacy in orthopaedic surgeries has become a topic of interest. This systematic review identifies seven studies that compare LB as a periarticular injection to other local anesthetics in adults undergoing THA.10–16
Pain Scores
LB aims to provide analgesia for up to 72 hours.18 Looking at short-term (up to 72 hours after surgery) pain scores, studies that found no significant differences in pain scores had larger study samples than those that found a significant reduction.10,12–14,16 Two of the three articles that found no difference in pain in the short-term period reported a reduction in pain in the first 24 hours after surgery.12,16 Of these two studies, Yu et al. also found a faster time to ambulate to 100 feet within the LB group. However, the improved pain control in the immediate period did not translate to reductions in total opioid consumption. Both Feng et al. and Yu et al. found no significant differences in MMEs consumed between the LB and control groups.12,16 Asche et al. and Johnson et al. found that patients receiving LB had significant reductions in pain in the short-term period. Still, only Asche et al. reported a coinciding reduction in total opioid consumption.10,13 Johnson et al. and Perets et al. are Level I evidence that reported pain scores when comparing LB and control groups. Johnson et al. found a significant difference in pain scores in the short term, and Perets et al. found no difference.13,14 The overall evidence does not demonstrate a difference in pain scores between the two groups in the short time. However, the potential benefits of reduced pain in the first 24 hours after surgery and quicker times to ambulation warrant further investigation.
Total Opioid Consumption
The view on opioids in postoperative pain management has been shifting so that they are now not as integral as they were once thought to be. Multimodal analgesia has been shown to provide better pain control, and the efficacy of LB in reducing total opioid consumption was assessed in this systematic review.2 Four of the seven papers that reported total opioid consumption, all with a larger overall sample size, found no significant difference in total opioid consumption, measured in MMEs, between the LB and control groups.12–14,16 Of the three studies that did find reductions in total opioid consumption, Beacher et al. reported a statistically significant reduction in average daily MME requirement per day from 29.01 to 22.59.10,11,15 However, clinical significance was not found as the risk of an overdose for both groups remains the same when compared to patients consuming 1 to <20 MME per day.19 Level I evidence in this systematic review found no significant difference in total opioid consumption.13,14 The current literature does not find a meaningful difference in opioid consumption between the two groups.
Secondary Outcomes
Five papers compared patients’ mobility in the LB group to that of the control group using parameters such as Activity Measure Post-Acute Care (AM-PAC) and Short Form-36 (SF-36) Scores.10,12–14,16 Of these, only Yu et al. found a significant improvement in time to ambulating 100 feet in the LB group. Additionally, this study found a decrease in pain within 24 hours of surgery in the LB group compared to the control.16 Feng et al. also found a reduction in pain within 24 hours of surgery but no difference in AM-PAC scores between the LB and control groups.12 Asche et al. reported a significant reduction in pain up to 72 hours postoperatively in the LB group compared to the control but found no difference between the groups in mean distance walked on postoperative days two and three.10 The lack of consistent evidence for decreased time to regain mobility among those treated with LB compared to controls necessitates further research. Mixed evidence remains on whether incorporating LB decreases length of stay, as three studies found a significant reduction in LOS and four did not. All three studies reporting a reduced LOS had a reduction in LOS of <1 day. While there is a potential benefit to reduced costs with a LOS reduced by <1 day, the clinical benefit of this reduction is unknown.20 None of the three articles that reported the incidence of adverse events and readmission rates found a significant difference in the incidence of adverse events.13,14,16 The current literature does not demonstrate any effect on complication rates in THA with the use of LB as a periarticular injection. LB is relatively more expensive than the current local anesthetics used as periarticular injections. Non-liposomal bupivacaine, a common local anesthetic used for periarticular injections in THA, costs about $3 per dose, whereas LB costs around $334 per dose.21 Despite this disparity, of the three studies that reported total costs, two found no significant difference, and one found a significant cost reduction.10,14,16 Total costs included hospital costs accrued during length of stay such as room and board, pharmacy, laboratory testing, imaging, and operating room. The negligible effect on cost might be due to comparing the overall costs of THA, where the cost of the local anesthetic might be insignificant compared to the total healthcare cost.
More research, specifically randomized controlled trials, needs to be conducted to compare better the efficacy of LB to current standards of care. A meta-analysis with stricter inclusion criteria for the control groups will offer stronger evidence to support or undermine the use of LB as a periarticular injection in total hip arthroplasty. Cost-benefit analyses can also be conducted to determine whether the outcomes justify the expense. Another limitation of this analysis is that it does not fully evaluate the clinical benefits of the results reported by some studies.
CONCLUSION
In our opinion, this systematic review finds that in patients undergoing total hip arthroplasty, protocols using periarticular liposomal bupivacaine result in minimal benefits of reducing pain scores and total opioid consumption when compared to traditional bupivacaine or ropivacaine. Future randomized controlled trials should evaluate outcomes important to patients, such as satisfaction with pain control and rehabilitation after total hip arthroplasty, when comparing periarticular injections with liposomal bupivacaine to other local anesthetics. Cost-benefit analyses are also needed to justify replacing bupivacaine and ropivacaine with a more expensive liposomal bupivacaine.
Declaration of Conflict of Interest
The authors do NOT have any potential conflicts of interest in the information and production of this manuscript.
Declaration of Funding
The authors received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of Ethical Approval for Study
The manuscript does not require ethical approval to report its findings.
Declaration of Informed Consent
There is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify patients.
Acknowledgments
None