INTRODUCTION
Anterior shoulder dislocation is one of the most common sports-related injuries with a high rate of recurrent instability, up to 67%, especially when the patients are young and active.1–4 The recurrent instability might cause later complications and potentially result in osteoarthritis.5 Although operative treatment is expected to lower the risk, some young male patients show subtle or frank instability, presenting with pain and discomfort and potential long-term damage to the glenohumeral joint over time.6–9
Several procedures, including arthroscopic Bankart repair or open Latarjet surgery, can address recurrent anterior shoulder instability.10 A recent meta-analysis revealed that recurrent dislocation is half less likely after Latarjet but caused a six-time higher risk of infection.11 There were no significant differences in the Rowe score, the need for revision, screw-related complications, or the postoperative hematoma formation between these two procedures. As a surgical intervention to treat shoulder instability, arthroscopic Bankart repair has been the most commonly used procedure to re-establish near-normal anatomy.12,13 However, 54% have experienced shoulder instability after Bankart surgery in the long-term follow-up.14 When there is a large bony deficiency or irreparable soft tissue damage, the Bristow, Latarjet, and Eden-Hybinette procedures are usually recommended.15 By restoring the architecture of the anteroinferior rim, these procedures correct the glenoid defect and are associated with satisfactory clinical outcomes and a lower recurrence rate than Bankart repair.15 Latarjet surgery, consisting of a bone block procedure, has shown a high success rate for shoulder instability16 and is particularly effective with a large deficient glenoid.17 Arthroscopic Latarjet also showed potential for managing recurrent anterior shoulder instability, but its complication rate remained high, and only highly experienced shoulder surgeons should perform it.18 Because there are multiple risk factors for postoperative recurrence,19,20 the gold standard of treatment for recurrent instability is unclear. Still, most agree that surgery is the best way to address the problem and facilitate a return to activities or the sports field.1,5,21
The current study aimed to compare the recurrence rates following arthroscopic Bankart repair and open Latarjet surgery for recurrent anterior shoulder instability. As a secondary outcome, we aimed to compare the functional and pain scores with appropriate patient-reported outcome measures (PROMs).
MATERIALS AND METHODS
Study design
This retrospective case-cohort study compared two treatment options for recurrent anterior shoulder instability: arthroscopic Bankart repair versus open Latarjet surgery. STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) guidelines for observational studies are followed in the presentation of this study.22 Our institutional review board (IRB) approved this study, and all procedures performed follow the national research committees (ethic code: IR.MUMS.MEDICAL.REC.1398.422). Patients were called and invited after having informed consent.
Study Population
Between 2008 and 2020, all patients with recurrent shoulder instability treated with either of the two methods at our tertiary referral university hospitals were included. The criteria for inclusion were a documented recurrent anterior shoulder dislocation and age<50 at the time of the surgery. We excluded patients with less than one year of follow-up, posterior or multi-directional instability, with off-track and bi-polar lesions that necessitate remplissage, concomitant surgeries for fractures or rotator cuff, revision surgery, stiff shoulder, and patient denial to participate.
Outcome measures and data acquisition
The study’s primary outcome measures were the incidence of recurrent instability and surgery complications at the last follow-up.
Instability was defined as “redislocation” or “subluxation,” described by Imam et al..11 The term subluxation was used to describe the patient’s subjective experience of glenohumeral slipping or shifting, followed by either spontaneous reduction or manual joint resetting by the patient.23 Redislocation is any documented dislocation that requires reduction by a medical professional or a third party.
The patient’s function and pain were assessed using the Oxford shoulder score (OSS) and shoulder pain and disability index (SPADI) as secondary outcome measures. The OSS questionnaire is considered a patient-reported outcome measure (PROM) of shoulder pain and function, consisting of 12 questions with five levels of the Likert scale. Each question is scored between 0 and 4; the total score ranges between 0 (worst patient condition) and 48 (normal shoulder).24 The SPADI self-rating tool has demonstrated good responsiveness, reliability, and validity for shoulder pain and function studies. There are 13 questions on a 0–10 scale separated into two sections: pain (five) and disability (eight). Each of these is scored on a separate subscale, and an overall score is calculated from 0 (best) to 100 (worst).25–27
Baseline and demographic variables were also collected. Occupations were categorized into light work (unemployed, employee, freelance, lawyer, student, and housewife) and heavy work (manual worker, chef, livestock breeder, farmer, teacher, barber, military, and driver).
Surgical technique
Patients of two orthopedic shoulder and elbow surgeons (MH.E and AR.K) were included in this study. Arthroscopic Bankart repairs were only performed on shoulders with no significant bone loss (<15%). Alternatively, the Latarjet procedure was performed if the preoperative computed tomography (CT) scan showed a 15% bone loss on the glenoid side or 30-40% humeral head bone loss.28 Surgeries were performed under general anesthesia and after 2 grams of cefazoline in the beach chair position. In this study, the Bankart procedure was performed arthroscopically following the technique described by Chechik et al., without closing the rotator interval arthroscopically.29 A minimum of three suture anchors were used starting from 5:30 on the right or 6:30 on the left. We did not perform a remplissage procedure in any of these patients. According to the description elsewhere, the Latarjet procedure was performed following the original method.30 The graft was left intra-articular with no attempt to close or interpose the capsule. We used the superior 7 cm of the deltopectoral approach over the coracoid, split the subscapularis longitudinally at 2/3-1/3 distance, and palpated and protected the axillary nerve. We rotated the coracoid 90 degrees downward with no inward rotation and covered the anteroinferior glenoid. The coracoid was fixed using two cannulated partially threaded 4.0 mm parallel screws over washers.
Statistical analysis
Results were summarized in tables by frequency (percentage) for categorical variables and mean + standard deviation (SD) for continuous variables. The Shapiro-Wilk test was used to test the normal distribution of the data. The student’s t-test or Mann-Whitney U test compared the continuous variables based on the normality. Also, the chi-square or Fisher’s exact test was used to compare the nominal variables. P-values of <0.05 were considered significant.
RESULT
In total, 133 patients (118 male, 89%) were included with recurrent instability, of which 67 underwent Latarjet and 66 underwent Bankart repair surgery [Table 1]. Patients in the two groups were similar in surgery side, hand dominance, education level, occupation difficulty level, and smoking status (P>0.05). However, patients in the Latarjet group were younger (32 ± 9 vs. 35 ± 9, P=0.04), with a higher male-to-female proportion (96% vs. 82%, P=0.01), and significantly shorter follow-up (3.2 ± 2.6 vs. 6.4 ± 3.0 years, P<0.001) than Bankart group.
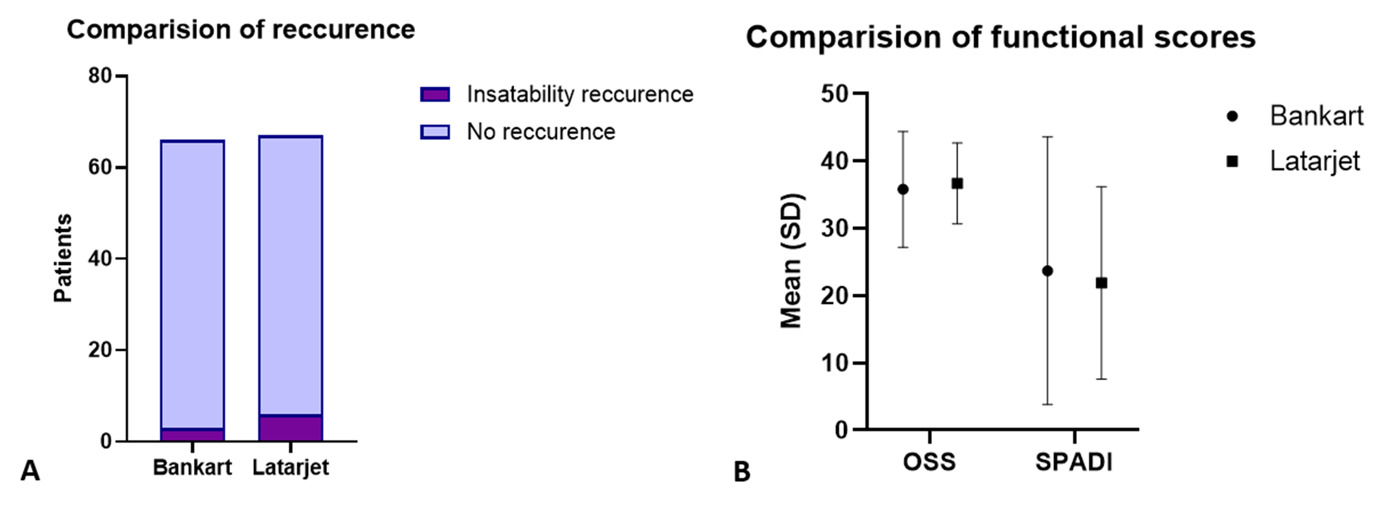
Only one patient in the Latarjet group experienced a recurrent dislocation (0.8% of total patients); however, the difference was insignificant between the groups (P=1.0). Three (4.5%) patients in the Bankart and five (7.5%) patients in the Latarjet group reported a subluxation, although the difference was not significant (P=0.72). Overall, instability (subluxation+dislocation) was higher in the Latarjet group but did not significantly differ (9% vs. 4.5%, P=0.49). No infection necessitating intervention was found (P=1.0). No nerve injury was detected after surgery in either group. [Table 2, Figure 1]
Both groups showed comparable pain and functional scores regarding OSS and SPADI total scores and their subscales (pain and disability) [Table 2, Figure 1]. The association of postoperative PROMs and patient characteristics was represented separately for the Bankart and Latarjet groups in Tables 3 and 4. In the Bankart group, both OSS and SPADI were significantly better in males. In addition, both OSS and SPADI scores improved significantly over time with the longer follow-up (P<0.05), and patients had more satisfaction, less pain, and better performance over time [Table 3].
In the Latarjet group, the total SPADI score was significantly better in patients with higher educational levels (19 ± 14 vs. 25 ± 14, P=0.045) than in patients with no university degree; however, other PROMs did not show a significant difference (P>0.05). In this group, younger age was significantly correlated with better outcomes (P<0.05) except for the pain subscale of SPADI (P=0.14) [Table 4]. Other factors, including sex, surgery side, occupation, and follow-up period, were not associated with the variation in PROMs in the Latarjet group.
DISCUSSION
This study’s main finding is that arthroscopic Bankart and open Latarjet resulted in low recurrence, few complications, and acceptable functional outcomes. This study observed that OSS and SPADI scores in the Latarjet group were 37 and 22, respectively, and in the Bankart group, they were 36 and 24, respectively, which was statistically insignificant. Male gender and younger age in the Latarjet group and time passed from the surgery in the Bankart group were associated with better performance and less disability. Both types of surgery were equally effective at improving symptoms, reducing instabilities, and improving patient satisfaction in their specific populations. Therefore, patients with minimal bone loss who are concerned about the disruption of shoulder anatomy in terms of aesthetic and occupational concerns may benefit from less invasive methods such as Bankart. Furthermore, the Latarjet procedure seems to have worked well for young and active patients with more glenoid bone loss since the superior outcomes were significantly correlated with younger ages in the Latarjet group.
This study faced some unavoidable limitations. Since the procedures were selected retrospectively, no randomization was possible, and it was not a matched cohort study. The assignment of patients with bone loss to Latarjet and no bone loss to Arthroscopic Bankart is a major flaw in this study. Moreover, the radiological evaluation of patients for degenerative joint disease was not performed. While additional assessments may have been valuable, our interview results and PROMs were appropriate for answering our primary study questions. Also, the baseline characteristics of the study’s groups were not similar in age, gender, and follow-up period. Lastly, a short follow-up period can undermine the study’s quality. This instability can return later, as well as progressing glenohumeral joint degeneration.
Our findings should be interpreted in light of the current indications for each technique based on bone loss, which is directly related to the number of dislocation episodes. Intuitively, a less invasive Bankart surgery shortly after a recurrent shoulder dislocation provides comparable outcomes with the open Latarjet in patients with long-standing conditions. When patients with recurrent dislocation are consulted to choose between operative versus non-operative management, this data shows that we can expect similar outcomes with early Bankart or later Latarjet surgery. Still, the difference entails the cosmesis of incision and a higher risk of complications and infection after Latarjet.
In a recent meta-analysis by Imam et al. on 7 cohort studies and 3275 shoulders,11 they revealed a higher risk of instability recurrence for the arthroscopic Bankart repair (Relative Risk (RR)= 2.9; 95% CI= 1.9-4.3; P<0.001). In this regard, only one randomized clinical trial has compared the arthroscopic Bankart with the open Latarjet procedures in the young male population with anteroinferior instability.2 After two years of follow-up, the risk of short-term postoperative redislocation after Arthroscopic Bankart is higher than that of open Latarjet (21% vs. 2%, P=0.006). Long-term follow-ups (6-10 years) showed that Latarjet was even more preferred in terms of recurrence of instability (RR= 3.0; 95% CI= 1.98-4.6).11 In contrast and in line with our study, some studies did not find a significantly different rate of redislocation and instability recurrence between groups.31 The findings of Cho et al. in a survey of patients with a large engaging Hill-Sachs lesion suggest that both the remplissage with Bankart repair and the Latarjet have similar recurrence rates (5.4% vs. 5.7%, P>0.05).31 Horinek*.*'s study with a similar design approved their findings.32 Their study differed from ours in that we performed isolated Bankart without remplissage because of the minimal bone loss.
Regarding PROMs, most previous studies reported similar scores for both techniques, as in our study.2,11,32 PROMs have three aspects: stability, function, and movement. Even though the stability component of the Latarjet was shown to be superior in some previous studies, the overall scores might not differ significantly when the function and mobility components are also considered.11 In contrast, some studies claimed superiority in one of the groups regarding subjective ratings.21 Zimmermann et al. demonstrated that even though the Latarjet group had a lower preoperative subjective shoulder value (SSV), they improved significantly more than the Bankart group and had higher SSV after surgery.21
A meta-analysis of complications by Williams et al. Shows an arthroscopic soft tissue repair complication rate of 1.6% and an open bone block operation complication rate of 7.2%.33 As bone block stabilization procedures are becoming more popular, including arthroscopic ones, surgeons must be aware of the 10-fold increase in complications.11,31,32,34 The arthroscopic Bankart procedure was associated with less infection risk than the Latarjet procedure, according to data pooled from three studies (RR, 0.16; 95% CI, 0.06-0.43; P<0.001).11,35–37 Hematomas and screw fixation complications were similar across groups.11 Our study did not identify any major complications, as expected, given the low rate of these procedures’ complications.
CONCLUSION
Our findings suggest that both Bankart and Latarjet are reliable techniques in short to mid-term follow-up based on the glenoid bone loss cut-off of 15%. The results may provide a clue for future research and suggest that patients can be consulted regarding early arthroscopic intervention soon after the shoulder dislocation becomes recurrent in contrast to waiting too long and causing significant glenoid bone loss to require more extensive surgery, albeit with comparable outcomes.
Declaration of conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Declaration of funding
There is no funding source for authors to declare
Declaration of ethical approval for study
All procedures performed in studies involving human participants were in accordance with the ethical standards of the National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards (Ethic code: IR.MUMS.MEDICAL.REC.1398.422).
Declaration of informed consent
An informed consent signed by all the study participants.
Acknowledgments
None