INTRODUCTION
Trapeziometacarpal joint, also known as first carpometacarpal (CMC1) joint, arthritis is a debilitating, yet frequent condition encountered within hand surgery. Patients who fail conservative management may pursue surgical intervention to improve pain, range of motion, and hand function.1,2 There are a myriad of surgical options available for the treatment of CMC1 arthritis. Early arthrosis may be treated with first metacarpal extension osteotomy, arthroscopic debridement, joint distraction, or interposition fat grafting. Late-stage arthrosis is usually treated with partial or complete resection of the trapezium, which can be modified to include hematoma distraction arthroplasty (HDA), ligament reconstruction (LR), tendon interposition (TI), suspension arthroplasty, or a combination of the aforementioned techniques.3 Other modalities include implant arthroplasty and arthrodesis. Trapeziectomy with ligament reconstruction and tendon interposition (LRTI) remains the most popular treatment choice amongst hand surgeons in the United States.4,5
Surgical interventions for CMC1 arthritis are frequently documented in the literature. Nevertheless, there remains uncertainty regarding which technique is superior. Prior studies comparing outcomes either do not address surgical indications, fail to recommend treatment based on patient demographics, or are relatively outdated, considering that CMC1 management is continuously evolving.6–8 This article aims to provide a single reference describing the most common treatment options, their indications, and their comparative outcomes.
SURGICAL MANAGEMENT
FIRST METACARPAL OSTEOTOMY
Thumb metacarpal osteotomy involves a 20° to 30° dorsal wedge closing osteotomy, also referred to as a thumb extension osteotomy, in the metaphysis of the thumb. The osteotomy is then stabilized with Kirschner wires (K-wire), plates, or screws, and the thumb is immobilized postoperatively until the osteotomy site is healed.9 The premise behind the procedure is that arthrosis usually begins volar and ulnar, near the beak ligament, and progresses dorsal and radial.10 The osteotomy corrects the adduction deformity and redistributes axial-loading forces from the volar to the dorsal.9,11 Therefore, the first metacarpal osteotomy is recommended for patients with early CMC1 arthrosis with dorsally intact cartilage. It may serve as a temporizing modality in younger patients as it allows for subsequent reconstructive procedures.9 Thumb extension osteotomy is relatively contraindicated for patients with moderate or advanced arthrosis as the osteotomy would then redistribute forces to denuded bone and would unlikely improve pain and function.
TRAPEZIOMETACARPAL ARTHRODESIS
Trapeziometacarpal arthrodesis (TMA) of the thumb is typically performed by fusing the metacarpal in approximately 45° of radial and palmar abduction and slight pronation to allow an opposable thumb to all four digits [Figure 1].12 Rigid fixation is performed using K-wires, tension band fixation, staples, headless compression screws, and/or plates and screws in isolation or combination.12–14 The CMC1 joint is immobilized until clinical and radiographic union.12 This technique is typically considered for advanced CMC1 osteoarthritis in active, young, high-demand individuals and manual laborers who require a stable joint.12,15 Relative contraindications include STT or pantrapezial arthritis, an unstable metacarpophalangeal joint, or an inability to tolerate a fixed trapeziometacarpal joint.12
TRAPEZIECTOMY
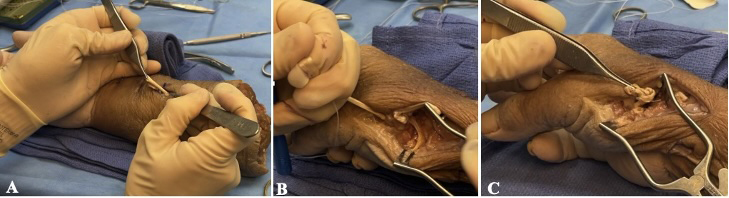
For patients with advanced pantrapezial disease, surgical management typically begins with a resection arthroplasty, first described by Gervis in 1949.3,16 The technique initially involved complete excision of the trapezium [Figure 2]. However, partial resection can also be performed. Trapeziectomy can be performed arthroscopically17 or open, and in isolation or concomitantly with an interposition or suspensionplasty.
HEMATOMA DISTRACTION ARTHROPLASTY
Resection arthroplasty alone may result in metacarpal subsidence. Alternative procedures have been proposed to maintain a larger arthroplasty space following trapeziectomy. Hematoma distraction arthroplasty (HDA) is postulated to increase joint space by suspending the thumb metacarpal until a cicatrix has formed within it [Figure 3].18 The thumb is distracted and secured in approximately 30° abduction and slight opposition by placing a K-wire into the base of the thumb metacarpal and either the index metacarpal, trapezoid, or scaphoid.18 The joint space is initially maintained by hematoma formation followed by dense scar tissue. Hematoma distraction arthroplasty has mostly been performed for patients with Eaton classification stage III and IV CMC1 arthritis.19,20
TRAPEZIECTOMY WITH LIGAMENT RECONSTRUCTION AND/OR TENDON INTERPOSITION
Additional methods for maintaining the joint space following trapeziectomy include ligament reconstruction (T+LR), tendon interposition (T+TI), or both (T+LRTI) [Figure 4]. Trapeziectomy +LR recreates the first intermetacarpal ligament, commonly using the flexor carpi radialis (FCR).21 The tendon is incised proximal to its insertion, passed through an intraosseous tunnel at the base of the thumb metacarpal, tensioned, and then secured to the periosteum.22 Other techniques incorporate the abductor pollicis longus (APL) or utilize allograft or xenograft.6 Alternatively, T+TI involves interposing a ball of tendon, most commonly from the FCR, APL, or palmaris longus (PL), within the joint space between the thumb metacarpal and scaphoid.6,23 Ligament reconstruction with tendon interposition combines both techniques, utilizing a tendinous graft to suspend the metacarpal and to interpose the joint space.23 Ligament reconstruction with or without tendon interposition can be performed for patients with advanced arthrosis who have low demands for thumb strength and are compliant with postoperative care.22 Contraindications include patients with active infection, instability of the CMC1 joint without arthrosis, and noncompliant patients.22 Additionally, these procedures may be relatively contraindicated in heavy laborers due to the potential for symptomatic laxity and loss of strength.13
SUSPENSION ARTHROPLASTY
Suture suspension arthroplasty (SSA) involves a hammock-like construct where a nonabsorbable braided suture is woven between the FCR and APL tendons to suspend the thumb metacarpal [Figure 5A].3,24 It preserves the joint space while limiting migration and subluxation of the metacarpal.3 Suture button suspensionplasty (SBS), also referred to as TightRope suspensionplasty, is an alternative technique that places a suture button between the base of the thumb and index metacarpal [Figure 5B]. It prevents proximal migration and abutment of the metacarpal against the scaphoid or partial trapezium without requiring a donor tendon.25 Both procedures are indicated for Eaton stages III and IV arthritis. While it can be performed for mild arthrosis, most surgeons prefer to utilize a method that only disrupts the distal trapeziometacarpal articulation.26
IMPLANT ARTHROPLASTY
Implant arthroplasty is an alternative option that is more commonly used internationally.27 Implant designs range from total joint replacements to hemiarthroplasties, interposition implants with partial or complete trapeziectomy, and interposition implants without trapeziectomy.28 Original implant materials had high complication rates involving instability, immunological reactions, and material failure.27 Currently, the most common implants are the total CMC prosthesis (TCP) and pyrocarbon implants.27 Implant arthroplasty may be indicated in the setting of advanced CMC1 arthritis without involvement of the scaphotrapeziotrapezoid joint.29
TRAPEZIOMETACARPAL JOINT DISTRACTION
Joint distraction is a relatively new joint-preserving technique that can help prevent the progression of arthritis through partial unloading of the joint surface.30 The technique involves inserting two K-wires in the trapezium and first metacarpal and then inserting a distractor device to distract the trapeziometacarpal space.31 The distractor remains in situ for eight weeks postoperatively.31,32 Joint distraction can be used in moderate to advanced CMC1 arthritis.32 Due to the novelty of this procedure for treating CMC1 arthritis, clear contraindications have not yet been established. However, patients over 65 years old and those with severe disease, prior surgeries involving the CMC1 joint, joint laxity, and/or inflammatory arthropathy were excluded from these early studies.30,31
OUTCOMES
In early CMC1 arthritis or ligamentous laxity, some surgeons may perform a thumb extension osteotomy as a temporizing modality in younger patients.9 However, these patients are at risk for pin-site-related infections. In a retrospective study of 32 metacarpal extension osteotomies, 28% had pin-site complications ranging from erythema to superficial infections requiring antibiotics. Two of those patients progressed to osteomyelitis, requiring formal debridement.9 These complications may also be inherent to other K-wire modalities, such as HDA. Alternative fixation modes may decrease the infection rate, including plating, staples, tension band constructs, and buried K-wires.9
Opponents of trapeziectomy performed in isolation propose that loss of the joint space can lead to pseudoarthrosis, adduction collapse deformity, and reduced function.3,16 However, patients with trapeziectomy have similar rates of osteoarthritis in adjacent carpal joints compared to wrists with an intact trapezium at an average of 17 years postoperatively.33 Additionally, initial improvements in functional and patient-reported outcome measures are sustained at long-term follow-up of 8.2 years compared to propensity-matched preoperative patients.16 In a systematic review of trapeziometacarpal joint arthritis, trapeziectomy in isolation was moderately to vastly superior in reducing the number of adverse events compared to T+LRTI with ½ FCR and T+LRTI with APL-FCR-APL.6 Despite concerns of metacarpal subsidence, isolated trapeziectomy provides satisfactory pain relief16 and reduced complications compared to LRTI.6
Arthroscopic hemitrapeziectomy improves patient-reported outcomes, pain, and grip and pinch strength at one year postoperatively.34 A randomized controlled trial of 62 thumbs demonstrated similar patient-reported outcomes and range of motion compared to open hemitrapeziectomy.35 However, partial trapeziectomy performed arthroscopically resulted in longer operative time,35 which can be attributed to an initial learning curve associated with its use. Despite this, arthroscopic trapeziectomy is a less invasive procedure that provides satisfactory outcomes.17
Trapeziectomy +LRTI using FCR significantly improves patient-reported outcomes at short- and long-term follow-up.23,36 Komura et al. demonstrated that grip and pulp pinch strength initially decreased at three months but significantly improved by 12 months postoperatively, while pulp pinch chronologically increased at final follow-up at a median of five years.23 Compared to T+LR using ½ FCR, a systematic review found that T+LRTI using ½ FCR demonstrated largely inferior outcomes in terms of physical function.6 However, compared to T+TI using PL, T+LRTI using ½ FCR was moderately superior in improving pain .6
Unlike other joint-space maintaining techniques such as T+LRTI, SSA, and SSB do not require donor tendons and thus avoid any associated donor-site morbidity.24 They both significantly improve pain postoperatively at short- and long-term follow-up.2,3,24 In a retrospective review of 90 SSA via the Wagner approach, DelSignore et al. found significant improvements in grip strength, key pinch, and tip pinch in addition to good-to-excellent improvement in pain relief at an average of 12.6 years postoperatively.3 However, postoperative complications included radiographic subsidence, recurrent metacarpal subluxation deformity, and FCR rupture.3 An additional complication associated with SSA includes irritation of the dorsal branch of the radial nerve.24 Significantly improved pinch strength and thumb range of motion are also documented for SSB.2 Suture suspension arthroplasty, and SSB share similar complications. However, SSB is associated with symptomatic hardware that may require revision in select cases2,25,37 as well as peri-implant fractures.25
Despite various designs and materials, implant arthroplasty has an overall higher failure rate compared to non-implant modalities, specifically trapeziectomy, T+LR, T+LRTI, and TMA.28 Hamasaki et al. demonstrated that implant arthroplasty, specifically a hemiarthroplasty implant, had moderately-to-largely inferior pain relief, functional improvement, treatment satisfaction, and adverse events compared to T+LRTI with ½FCR-APL-½FCR, T+ LRTI with APL-FCR-APL, and trapeziectomy by posterior approach.6 Complications include persistent pain, aseptic loosening, dislocation, periprosthetic fracture, subluxation, and osteolysis.28 When analyzing specific implants, Ganhewa et al. found that interposition implants with complete trapeziectomy had the lowest failure rate, and interposition implants with partial or no trapeziectomy had the highest failure rates within the implant arthroplasty group.28 Alternatively, in a prospective case series of 166 total joint arthroplasty implants, Cootjans et al. demonstrated an implant survivorship of 96% at a mean follow-up of 80 months,38 suggesting that implant arthroplasty may be emerging as a reliable treatment option. However, further prospective studies are required.
Outcomes following TMA vary throughout the literature. Despite concerns of sacrificing motion, patients with advanced CMC1 arthritis with concomitant hyperextension deformity may sustain their total functional range of motion postoperatively.39 Hayashi et al. found that active metacarpophalangeal joint flexion increased while extension decreased, resulting in a similar functional arc of motion postoperatively.39 Additionally, Hippensteel et al. showed that TMA resulted in significantly increased thumb opposition and metacarpophalangeal motion compared to T-LRTI, likely from compensation of the scaphotrapezial joint.13 Trapeziometacarpal arthrodesis is associated with improved patient-reported outcome measures,13,14 pain,13,14 and grip strength14 postoperatively. However, in a systematic review of 914 TMA, Dharamsi et al. reported a complication rate of 48.7%, with 15.1% requiring reoperation, most commonly for symptomatic hardware (8.6%) and nonunion (4.3%).14 Compared to T+LRTI with ½ FCR-APL-½ FCR, Hamasaki et al. found that TMA was largely inferior in relieving pain, improving physical function, and reducing adverse events.6
Trapeziometacarpal joint distraction is relatively new; therefore, outcomes are not well-described in the literature. In a prospective case series of 20 patients with stage II and III CMC1 arthritis, Ottenhoff et al. demonstrated significant improvements in Disabilities of the Arm, Shoulder, and Hand and Visual Analogue Scores at an average of two years postoperatively following CMC1 joint distraction.31 Spaans et al. also found improvement in patient-reported outcomes at one year following CMC1 joint distraction.32 Complications, such as pin-site infections and hardware failure, are inherent to using K-wires.31 Although promising, further studies are needed to assess long-term outcomes following joint distraction.
CONCLUSION
Trapeziometacarpal joint arthritis is a debilitating condition frequently encountered in hand surgery. Patients who fail conservative treatment may pursue surgical intervention. Metacarpal extension osteotomy can be considered in young patients with early-stage arthritis. Patients with advanced CMC1 arthritis may undergo partial or complete trapeziectomy, which can be augmented with HDA, LR, TI, LRTI, or suspension arthroplasty. Young manual laborers with advanced arthritis may benefit from trapeziometacarpal arthrodesis. Alternative options include implants and joint distraction. Current literature demonstrates comparable outcomes among the different procedures with inconsistent results regarding the superiority of one technique over the other. Therefore, treatment should be tailored based on the patient’s symptoms, stage of arthrosis, and surgeon experience. Further research is recommended to directly compare indications, contraindications, and outcomes using randomized controlled trials.
Declaration of conflict of interest
The authors do NOT have any potential conflicts of interest for this manuscript.
Declaration of funding
The authors received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of ethical approval for study
This manuscript does not require ethical approval to report its findings.
Declaration of informed consent
There is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify patients.

_anteroposterior__(b)_oblique__and_(c)_lateral_radiographs_demonstrating_a_trapeziometa.png)
_cadaveric_image_depicting_a_complete_trapeziectomy_(b)_and_the_remaining_joint_space.png)



_anteroposterior__(b)_oblique__and_(c)_lateral_radiographs_demonstrating_a_trapeziometa.png)
_cadaveric_image_depicting_a_complete_trapeziectomy_(b)_and_the_remaining_joint_space.png)